Original article
Published in spanish Científi ca Dental Vol. 21. Nº 1. 2024
www.cientificadental.es
From mild COVID to long COVID: comprehensive oral health assessment
Introduction: COVID-19 has caused a wide range of symptomatology, including that present in the oral cavity. A new related syndrome is gaining importance: Long COVID. The aim of this work is to analyse the effect of SARS-CoV-2 infection at the oral level in subjects diagnosed with Long COVID, compared to acute infection.
Methods: A case-control study was conducted with 102 subjects recruited between 2021 and 2022, from whom 34 oral health variables and possible risk factors were obtained.
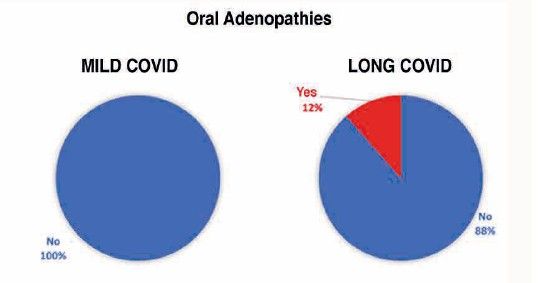
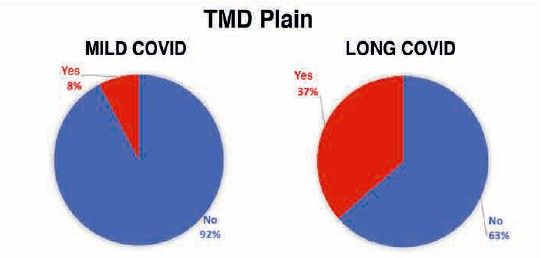
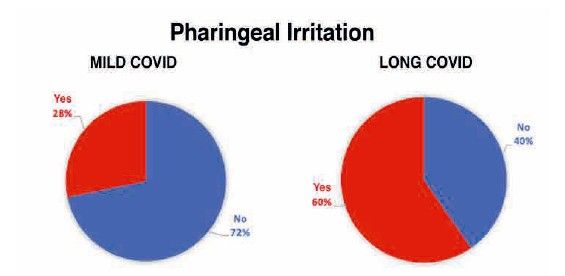
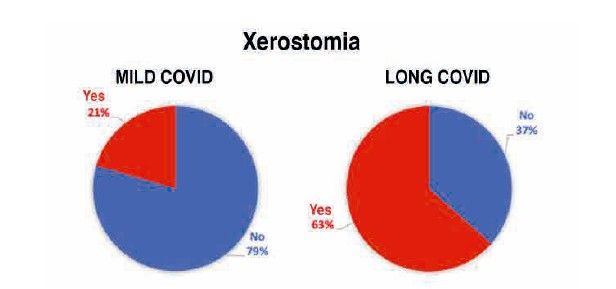
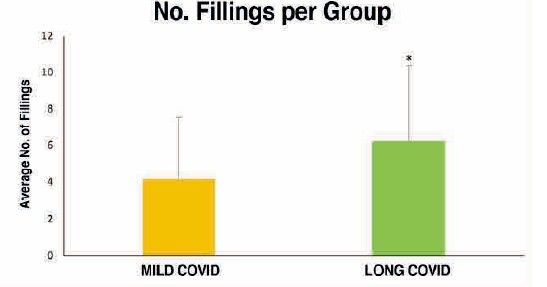
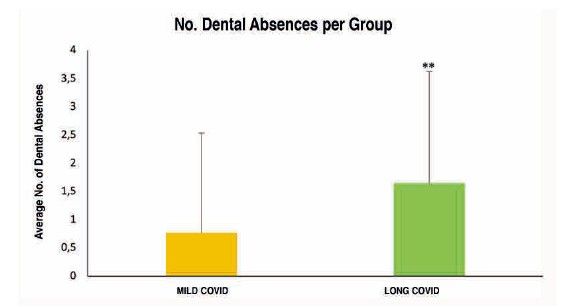
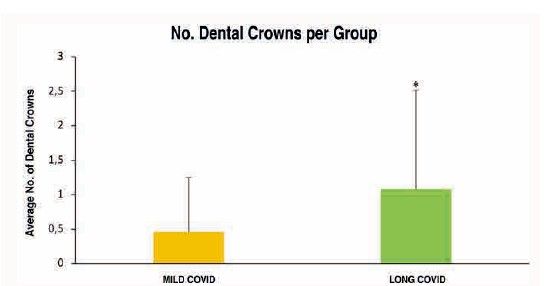
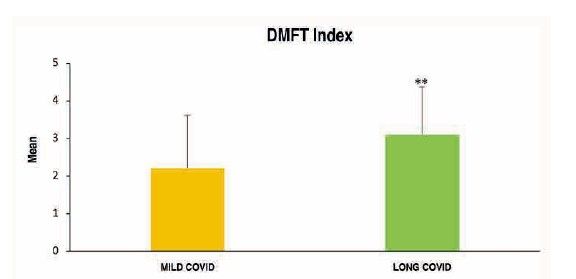
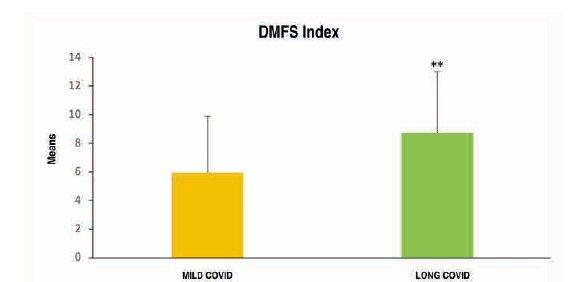
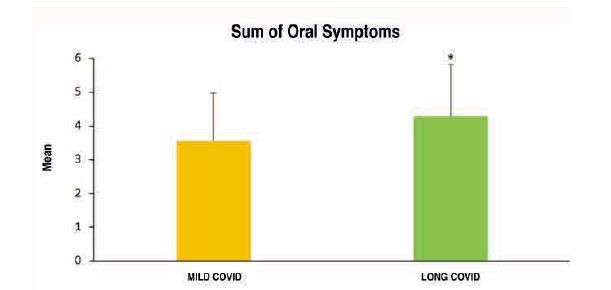
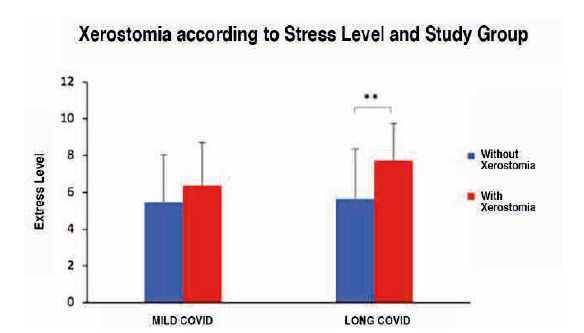
Results: Statistical analysis revealed that Long COVID subjects had significantly higher prevalence of: adenopathies, TMJ pain, pharyngeal irritation, xerostomia, fillings, dental absences and dental crowns, higher CAOM and CAOD index values and higher total dental symptoms. In addition, stress appeared as a risk factor; those patients with Long COVID who presented a higher level of stress (7.73 ± 2.02) were also those who suffered, to a greater extent, from xerostomia or bruxism, responsible for TMJ pain, also more prevalent in this group.
Conclusions: Long COVID causes oral manifestations related, some of them, to the fact that the oral cavity is a route of entry of the virus, such as mucosal irritation; others, related to its possible autoimmune nature, such as mucosal irritation; others, related to its possible autoimmune nature, such as xerostomia and, in the same way, others related to stress, reflected in the presence of bruxism. It is essential to develop protocols that improve both the early diagnosis and management of these patients in our clinics.
Key words: COVID-19; Long COVID; Mucosal irritation; Xerostomia; Adenopathies; Bruxism and stress.
The impact of the COVID-19 pandemic was profoundly transformative for humanity, affecting every aspect of our lives. When, at the end of 2019, the SARS-CoV-2 virus altered its evolution to make the leap to the human host, no one could have imagined the repercussions this would entail. Since the first cases were identified at the end of 2019, the virus spread rapidly worldwide, generating an unprecedented health crisis.
This is a highly contagious virus that has raised significant questions regarding community transmission processes, the pathogenesis of infections, and, above all, its involvement in the immune response. The latter was the catalyst for investigations that revealed how COVID-19 can exacerbate pre-existing autoimmune diseases and may trigger an exaggerated immune response in certain patients, thereby worsening the clinical picture1.
Indeed, a proportion of infected individuals continue to manifest disease-related symptoms, of variable intensity, persisting over time. This proportion varies depending on the state of chronic inflammation prior to infection and the pre-existing diseases of each individual, although data published by the World Health Organization, as of March 2023, appear to indicate that approximately 10% to 20% of the population experiences medium- and long-term effects following the initial infection. These cases have been classified within a new category termed ‘persistent COVID syndrome’, ‘post-COVID syndrome’, ‘post COVID-19 condition’ or ‘Long COVID’.
Long COVID can affect individuals of any age, sex, or medical condition and encompasses a wide range of clinical manifestations, which may involve various systems, including the cardiovascular, respiratory, and nervous systems2.
In general, it is believed that the underlying pathological mechanisms of Long COVID may be related to a state of chronic inflammation and tissue damage induced by the virus. These processes may generate an exaggerated residual inflammatory response, which can result in organ damage and prolong the recovery of patients. Furthermore, the immune response may account for Long COVID, as some patients have demonstrated a hyperactive and sustained immune response following infection, which may result in chronic inflammation and persistent organ damage3.
Within the context of the pandemic, mechanisms related to stress cannot be disregarded. It should be understood, in principle, as a natural physiological and psychological response of the organism to adverse situations, constituting a natural protective mechanism. However, when such stress is prolonged, it may have detrimental effects on health4. In recent years, it has been demonstrated that chronic stress can affect the immune system and predispose individuals to the development of infectious diseases. This is attributable to the fact that stress can alter the immune response, modifying its capacity to combat infectious agents and thereby diminishing its competence to protect against diseases5.
Finally, COVID-19 has caused a wide range of symptoms and complications across various bodily systems. Among others, a wide variety of oral symptoms have been reported, which must be addressed to ensure appropriate diagnosis and treatment of these patients6. However, it is important to emphasise that these oral manifestations associated with COVID-19 are not specific to this disease, but may also occur in other conditions, both infectious and non-infectious. They primarily present in the following forms:
• Oral lesions resembling recurrent aphthous stomatitis: these may be found in various areas within the oral cavity, including the buccal mucosa, lips, and palate7.
* Oral ulcers: similar to those observed in other viral infections such as herpes simplex virus (HSV) and Epstein-Barr virus8, and have even been considered an initial sign of COVID-199.
• Lesions on the tongue: similar to geographic tongue10.
• Necrotising ulcerative gingivitis: more common in patients with COVID-19 than in individuals without the disease11.
Alterations in taste perception (dysgeusia): as well as anosmia, related to the sense of smell. Patients infected with COVID-19 may experience a reduction in their sense of taste, alterations in flavour, or a complete loss thereof. The majority of patients exhibit these changes temporarily; however, some may experience this symptom as a persistent long-term effect following recovery from the disease12.
• Others: xerostomia, halitosis, vesiculobullous lesions, fissures or depapillation of the tongue, and oral candidiasis13.
All these manifestations may be of concern to patients with COVID-19 and to dental health professionals, as they could indicate an active infection and the need for appropriate follow-up. Studies have demonstrated that SARS-CoV-2 is present in the saliva of infected patients from the early stages of infection and has also been detected in samples obtained from the tonsils, suggesting that the salivary glands may also serve as a potential reservoir for the virus. This could be due to the high expression of ACE2 receptors in the salivary glands14, a demonstrated entry point for the virus into cells. It has also been proposed that oral manifestations associated with COVID-19 may be related to dysfunction of the immune system15.
However, we found limited literature on oral health in patients with long COVID and the implications of the pandemic for the general population in this respect. Therefore, the objective of this study was to comprehensively evaluate the effect of SARS-CoV-2 infection on oral health status and, more specifically, its condition in individuals who developed long COVID.
The present study is a sub-analysis of a broader investigation focused on the pathophysiology of long COVID-19, approved by the ethics committee of the European University of Madrid (Internal code CIPI/20/207). All patients provided informed consent to participate prior to inclusion.
The definition of the study groups was as follows:
1. Case group: subjects diagnosed with long COVID-19. Sixty-three subjects, all adults, belonging to the Long Covid ACTS association of the Community of Madrid were recruited. None had active infection or severe systemic diseases in cases where examination is not recommended due to the life-threatening risk to the patient (ASA IV and V).
2. Control group: subjects who had experienced infection with the SARS-CoV-2 virus and either did not present with symptoms associated or whose symptoms resolved upon remission of the infection. Thirty-nine volunteer subjects were recruited via a social media campaign who met the inclusion criteria: over 18 years of age, from the Community of Madrid, and who had experienced the infection without sequelae.
The study was divided into two phases. In the first phase, the recruitment of the sample for both study groups was conducted, from September to November 2021. In the second phase, an oral examination and clinical interview of the subjects were performed.
This second phase was conducted at the University Dental Clinic of the European University of Madrid between November 2021 and April 2022. Before the clinical appointment, each patient completed a 20-item questionnaire covering demographic data, stress factors before and after infection, general health, and aspects related to SARS-CoV-2 infection. At the clinic, a full medical history and oral examination were performed, which included:
• Extraoral examination for the collection of data on pathologies and/or abnormalities such as tumours, cellulitis, adenopathies, cutaneous lesions, and asymmetries located in the head and neck regions.
• Assessment of temporomandibular joint (TMJ) status: degree of mouth opening, presence of articular clicks, deviation, and presence of pain on palpation during mouth opening and closure.
• Intraoral examination for the detection of soft tissue alterations (lips, buccal mucosa, tongue, floor of the mouth, retromolar region, palate, gingiva, and pharynx), evaluation of oral hygiene status (OHI-S index), recording of the number of carious lesions, obfillings, absences, fractures, root remnants, crowns, bridges, removable prostheses, as well as calculation of the DMFT and DMFM indices. Finally, periodontal status was assessed (probing depth, recessions, attachment loss, tooth mobility, furcation involvement) and the Community Periodontal Index of Treatment Needs (CPITN) was calculated.
Statistical analysis
For the descriptive study, relative frequencies were calculated for qualitative variables and, for quantitative variables, the mean and standard deviation were calculated.
In cases where the quantitative variables followed a normal distribution and were categorised by qualitative variables, parametric tests were performed. For variables with two categories, the Student’s t-test was performed; if the variable had three or more categories, Levene’s test for homogeneity of variances was conducted prior to ANOVA.
For those without a normal distribution, non-parametric tests were performed: the Mann-Whitney U test for variables with two categories, and the Kruskal-Wallis test for those with three or more.
Additionally, Pearson’s Chi-square test was applied in cases where the independence between two qualitative variables was analysed. Similarly, in these tests of independence, when the p-value is significant (p<0.05), we can accept the hypothesis with 95% confidence that there is a statistically significant difference in the mean value of the variable between the different groups.
All statistical tests were conducted with a 95% confidence level, and version 26 of the IBM SPSS statistical software was utilised.
The study was conducted on a total of 102 subjects, of whom 20 were men (20%) and 82 were women (80%), with ages ranging from 23 to 68 years.
By study group, there was a higher proportion of subjects in the mild COVID group within the 26 to 45 years age range. However, in the long COVID group, there was a greater number of subjects within the age range of 36 to 65 years.
To analyse the level of oral health in subjects with long COVID, 34 related variables were examined. Of all these oral health markers explored both extraorally and intraorally, and subsequently analysed according to the study group, the following were observed to a greater extent and with high statistical significance in the long COVID group (Table):
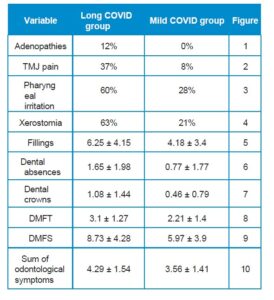
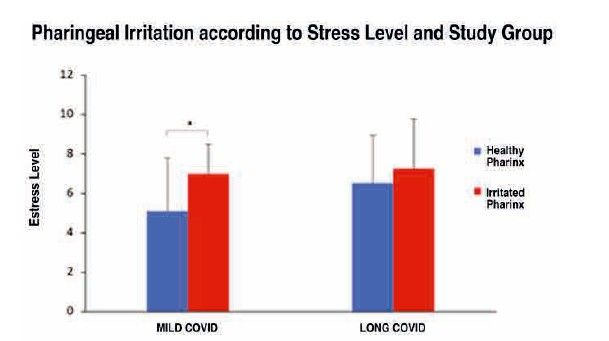
Stress was identified as one of the most influential factors in oral health. As shown in Figure 11, mild COVID subjects with a higher current subjective stress level (7 ± 1.48) also exhibited greater pharyngeal irritation compared to those with a lower stress level (5.11 ± 2.69) and consequently an unaltered pharynx, this difference being statistically significant.
However, this did not occur in subjects with long COVID because, although they exhibited higher levels of stress, the differences observed in pharyngeal irritation were attributable to chance.
Conversely, it is the long COVID study subjects with higher levels of stress (7.73 ± 2.02) who experienced greater xerostomia compared to those with lower levels (5.63 ± 2.73), this difference being significant according to the Mann-Whitney U statistic (p<0.01) (Figure 12).
Among the possible systemic conditions caused by the SARS-CoV-2 virus, it is necessary to analyse in depth its impact on the oral cavity. COVID-19 infection may give rise to various oral manifestations, primarily at the mucosal level. In the present study, it was observed that the number of dental symptoms—such as periodontal and peri-implant involvement, the presence of aphthae, mucosal irritation due to outbreaks, halitosis, dentine hypersensitivity, or the presence of caries—was higher in subjects belonging to the long COVID group. A possible explanation for this set of manifestations may be posited given that the oral cavity forms part of the upper respiratory tract and represents one of the potential direct routes for the entry of the SARS-CoV-2 virus, owing to the presence of ACE2 receptors in the oral mucosa and in the epithelial cells of the salivary glands16.
It should be emphasised that individuals who exhibited persistent systemic symptoms related to COVID-19 also presented certain oral manifestations, such as the presence of adenopathies, the subjective sensation of dry mouth (xerostomia), pharyngeal irritation, and temporomandibular joint pain as a consequence of bruxism. Of these, the presence of adenopathies, xerostomia, and mucosal irritation at the pharyngeal level are clinical manifestations that are likewise observed in certain autoimmune pathologies, such as Sjögren’s syndrome, rheumatoid arthritis, systemic lupus erythematosus, type I diabetes, or multiple sclerosis, among others17. This raises the possibility of an autoimmune nature for long COVID.
In the case of pain experienced at the level of the temporomandibular joint, generated by dental clenching, predominantly nocturnal, it may be closely related to the level of stress currently perceived by individuals with long COVID, largely due to their complex medical condition18.
Moreover, during the lockdown, dental clinics suspended their activities, limiting dental care solely to specific dental emergencies and, as far as possible, avoiding clinical treatments that generated aerosols19. This reduction in dental care, home confinement as a social distancing measure, the socio-economic crisis experienced, increased levels of stress, as well as anxious-depressive symptoms, together with the pathophysiological situation in which individuals with long COVID found themselves, complicated such a routine act as daily oral hygiene through tooth brushing and frequent visits to the dentist. This may account for the significant deterioration in oral health status observed in patients with long COVID, as evidenced by a higher number of restorations, missing teeth, crowns, and caries index in comparison with those with mild COVID.
Among the limitations, the biases of our study arise from the selection of cases from a single patient association, which hinders the extrapolation of the results. The imbalance between the number of cases and controls is also recognised, which was addressed through a multivariate analysis to adjust for variables that could affect the confidence level of the results. Robust studies are required to develop follow-up and control protocols at the onset of the disease, in order to evaluate the factors involved in resolution without sequelae or, conversely, in progression to long COVID.
Accordingly, the advancement of clinical practice in dentistry necessitates the promotion of research strategies that enable the expansion of our understanding of long COVID and its early diagnosis, as well as its prevention, potentially within the remit of dental professionals.
Individuals affected by long COVID demonstrate various related oral manifestations, some of which are attributable to the oral cavity serving as an entry route for the virus, such as mucosal irritation or the presence of aphthae; others to the possible autoimmune nature of this new syndrome, such as xerostomia or the presence of adenopathies, and, finally, other manifestations may be associated with stress, such as the presence of TMJ pain, indicative of bruxism.
Wang Y-H, Peng L, Jiang J-H, X, et al. Misdiagnosis of primary mucosa- associated lymphoid tissue lymphoma of the pleura: case report and literature review. Transl Cancer Res. 2022;11(9):3315–3321.
Carrillo-Esper R. Post-COVID-19 syndrome. Gac Med Mex. 2022;158(3).
Ding Y, Zhou Y, Ling P, et al. Metformin in cardiovascular diabetology: a focused review of its impact on endothelial function. Theranostics. 2021;11(19):9376–9396.
Pervanidou P, Agorastos A, Kolaitis G, Chrousos GP. Neuroendocrine responses to early life stress and trauma and susceptibility to disease. Eur J Psychotraumatol. 2017;8(sup4).
Kabré WLMEB-, Ouédraogo N, Coulibaly AC, et al. Phytochemical, antioxidant and anti-inflammatory effects of extracts from Ampelocissus africana (Lour) Merr (Vitaceae) rhizomes. J Pharm Res Int. 2020;8–18.
Klugar M, Riad A, Mekhemar M, et al. Side effects of mRNA-based and viral vector-based COVID-19 vaccines among German healthcare workers. Biology. 2021;10(8):752.
Pedrosa M da S, Sipert CR, Nogueira FN. Salivary Glands, Saliva and oral findings in COVID-19 infection. Pesqui Bras Odontopediatria Clin Integr.2020;20 (suppl 1).
Vigón L, García-Pérez J, Rodríguez-Mora S, et al. Impaired antibody-dependent cellular cytotoxicity in a Spanish cohort of patients with COVID-19 admitted to the ICU. Front Immunol. 2021;12.
Binmadi NO, Aljohani S, Alsharif MT, Almazrooa SA, Sindi AM. Oral manifestations of COVID-19: A cross- sectional study of their prevalence and association with disease severity. J Clin Med. 2022;11(15):4461.
Orilisi G, Mascitti M, Togni L, et al. Oral manifestations of COVID-19 in hospitalized patients: A systematic review. Int J Environ Res Public Health. 2021;18(23):12511.
Bermúdez Bermúdez M, Cuadro Montero KM, Parra Sanabria EA, Rueda Jiménez A, Peña Vega CP. Manifestaciones en la cavidad bucal y en la cara asociadas a la COVID-19. Univ Médica. 2021;62(3).
Kisiel MA, Janols H, Nordqvist T, et al. Predictors of post-COVID-19 and the impact of persistent symptoms in non- hospitalized patients 12 months after COVID-19, with a focus on work ability. Ups J Med Sci. 2022;127.
Stavem K, Ghanima W, Olsen MK, Gilboe HM, Einvik G. Prevalence and determinants of fatigue after COVID-19 in non-hospitalized subjects: A population- based study. Int J Environ Res Public Health. 2021;18(4):2030.
Malarvili MB, Alexie M, Dahari N, Kamarudin A. On analyzing capnogram as a novel method for screening COVID-19: A review on assessment methods for COVID-19. Life. 2021;11(10):1101.
Gaudin A, Badran Z, Chevalier V, et al. COVID-19 and Oral Fluids. Front Dent Med. 2020;1.
Lechien JR, Radulesco T, Calvo- Henriquez C, Chiesa-Estomba CM, Hans S, Barillari MR, et al. ACE2 & TMPRSS2 expressions in head & neck tissues: A systematic review. Head Neck Pathol. 2021;15(1):225–235.
Edwards M, Dai R, Ahmed SA. Our environment shapes us: The importance of environment and sex differences in regulation of autoantibody production. Front Immunol. 2018;9.
Dias D, Botelho H, Bortolotti AL. Dos Reis AC. Neuroscience contributes to the understanding of the neurobiology of temporomandibular disorders associated with stress and anxiety. Cranio. 2021;13:1–6.
Brian Z, Weintraub JA. Oral health and COVID-19: Increasing the need for prevention and access. Prev Chronic Dis. 2020;17(200266).

Sánchez Fernández, Sara
Graduate in Dentistry from the University of Zaragoza.
Master’s in Advanced Periodontics from the European University of Madrid. Doctoral student at the European University of Madrid.
García Guerrero, Iván
PhD in Dentistry from Rey Juan Carlos University.
Master’s in Oral Surgery and Implantology from Rey Juan Carlos University. Principal Investigator, Faculty of Biomedical Sciences, European University of Madrid.
Palomino Barrigas, Ana I.
PhD in Neuroscience from the Complutense University of Madrid. Collaborating Researcher, Faculty of Biomedical Sciences, European University of Madrid. Associate Lecturer, Affiliated Centre of Camilo José Cela University.