Clinical case
Published in spanish Científica Dental Vol. 19. Nº 2. 2022 www.cientificadental.es
Block grafting in combination with the two-stage split technique for the rehabilitation of a case of severe bone resorption of the maxilla in width
The use of different surgical techniques to achieve the resolution of the most complex atrophy cases is of vital importance.
Increasingly, we have cases with edentulism of longer duration in our practice that require implant treatment with fixed prosthesis, which is a challenge when planning and carrying out treatments. To do this, we can use different techniques that allow us to gain width and height, as well as implants of different lengths and diameters that allow us to adapt to each situation. In the present clinical case, we show a rehabilitation that combines different surgical techniques to achieve the desired result.
More and more frequently, patients with long-term edentulism, wearing complete prosthesis come for dental consultation requesting implantology treatment. The digital age, social networks and patient access to clinical information in dentistry, means that the latest advances in rehabilitation of extremely atrophic maxillary and mandible reach the patients and they demand a solution to their situation, they thought it could not be corrected in any other way than with removable dentures1-4. Therefore, patients sometimes request implantology treatments in cases of great complexity that make us have to use all the surgical and prosthetic tools at our disposal to solve them5.
When we face a severe resorption in a horizontal sense, both in the maxilla and in the mandible, there are different techniques that help us to recover the lost bone volume to later insert dental implants6-7. Each of the techniques has its indications and may, sometimes, in the same patient, need several of these techniques to achieve a regeneration of the lost bone volume, since there are substantial variations in the quality and quantity of bone volume within the same arch of the same patient, as well as areas where in addition to width the bone plates have been completely or partially lost, which changes the approach of the technique to employ6-9.
In general, when there is a reduced bone width (below 3 mm of residual crest) that does not allow direct insertion of the implant we can opt for an expansion or split crest, in one or two phases, as long as the two bone plates are available and there is a bone particulate between them that allows the separation between them by inserting the definitive implant or the expander implant10-14. When one of the two bone plates is absent, in that case, the recommendation will be to use block grafts or guided bone regenerations13-14.
Both techniques are widely documented15, and the selection between one procedure and the other is mainly based on the availability of autologous bone to perform block surgery, and the ability of the operator to perform the technique, since the use of blocks requires a greater learning curve and can lead to more complications in obtaining, manipulating and healing, since it is a technique of greater technical difficulty.
In spite of all this, if careful protocols are used to obtain the graft, and a careful positioning technique is performed, paying special attention to soft tissues, nowadays, it can be performed without greater rate of complications than the bone regeneration technique, especially when the intraoral area is used as the donor zone and the obtained bone is maximized by dividing the block as described by Khoury16-18.
In the following clinical case, a situation is shown where different procedures have been necessary to rehabilitate the maxilla with extreme bone loss in width, depending on each of the areas to be treated, individualizing the type of treatment according to the characteristics of the remaining bone recess.
We present the clinical case of a 56-year-old female patient, who has been wearing an upper complete removable prosthesis and a lower partial prosthesis for more than 20 years. She comes for consultation requesting implant rehabilitation to replace her current prosthesis to improve her masticatory function. In the intraoral examination we can observe that the prosthesis meets quite satisfactorily the aesthetic requirements of the patient, but according to her, they move when chewing. When removing the prosthesis, a maxillary edentulous ridge with an evident centripetal resorption that has left the starting situation close to that of a skeletal class III (Figures 1 and 2).
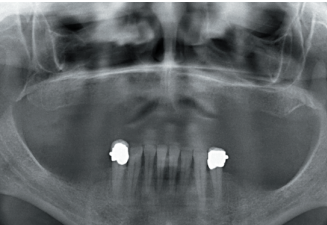
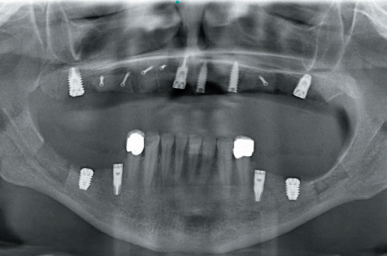
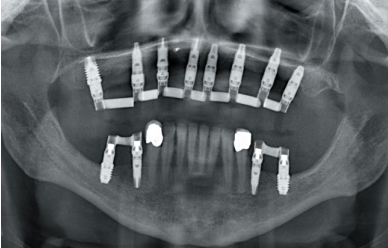
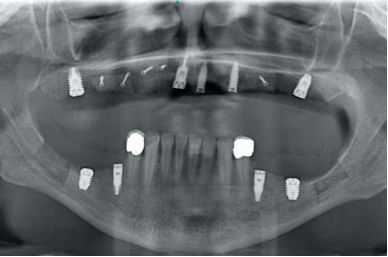
To start the diagnostic phase, a panoramic radiograph is performed that gives us an idea of the general condition of both jaws to start the treatment plan.
It shows that there is apparently some height in the maxillary ridge both anterior and posterior and a low dental nerve in the jaw that allows us to have a greater residual bone crest available for the insertion of the implants (Figure 3).
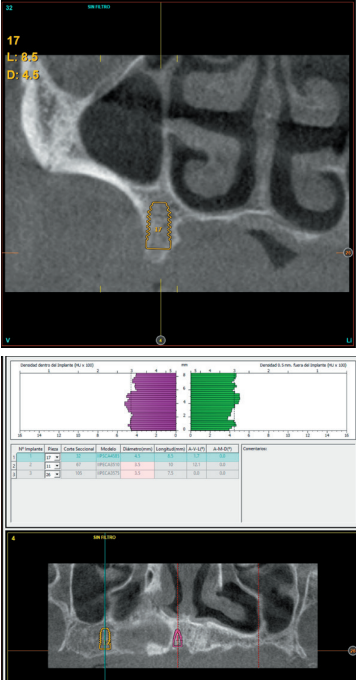
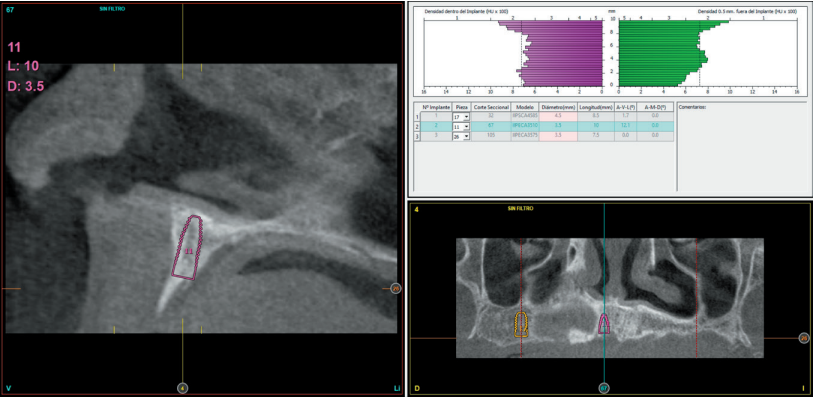
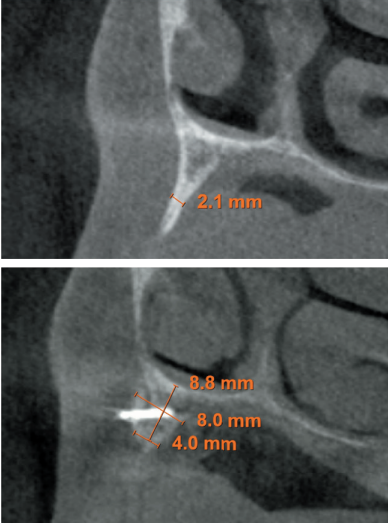
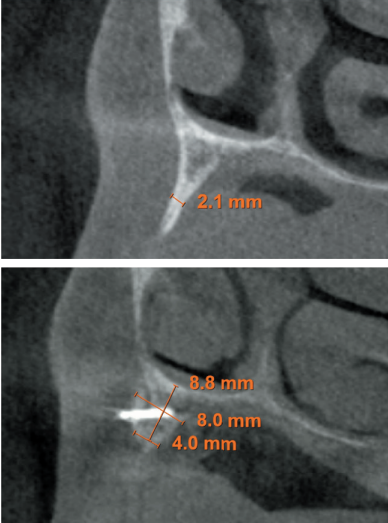
Subsequently, we proceed to perform a dental cone beam that offers a more accurate view of the type of implant rehabilitation that can be proposed. In the sections corresponding to the upper maxilla, there are areas where the direct insertion of the implants can be performed such as those corresponding to 16 and the central incisor zone of this quadrant (Figures 4-5) or in the second quadrant the area of the 27.

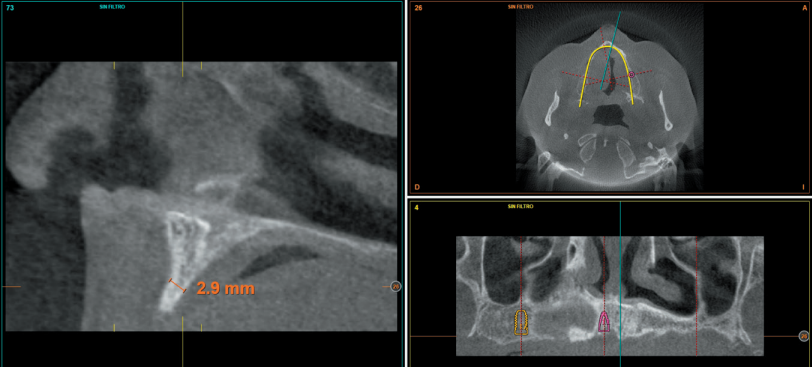
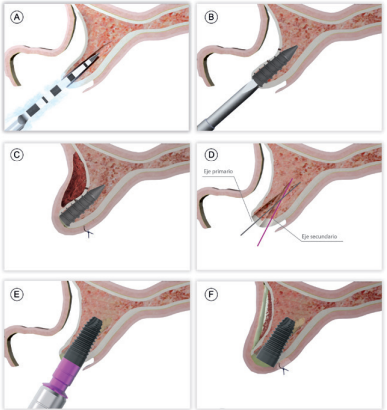
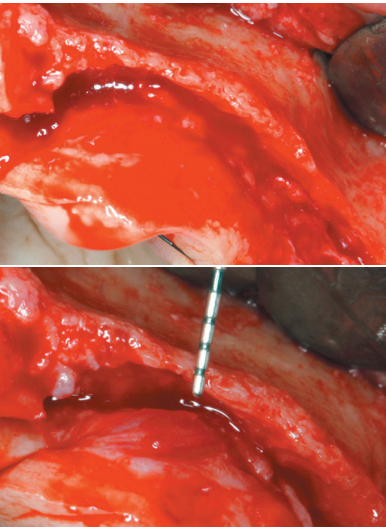
implant rehabilitation that can be proposed. In the sections corresponding to the upper maxilla, there are areas where the direct insertion of the implants can be performed such as those corresponding to 16 and the central incisor zone of this quadrant (Figures 4-5) or in the second quadrant the area of the 27. On the other hand, in the area corresponding to teeth 21 and 23 there is a significant horizontal atrophy, with a residual bone width of approximately 3.5 mm in the middle zone of the crest, with an enlargement in the most basal area of the same and conservation of both corticals. This leads to choose a split crest technique, in this case in two phases to achieve a greater final width and correct the inclination of the final implant as much as possible to achieve adequate aesthetics in the final prosthesis (Figure 6).
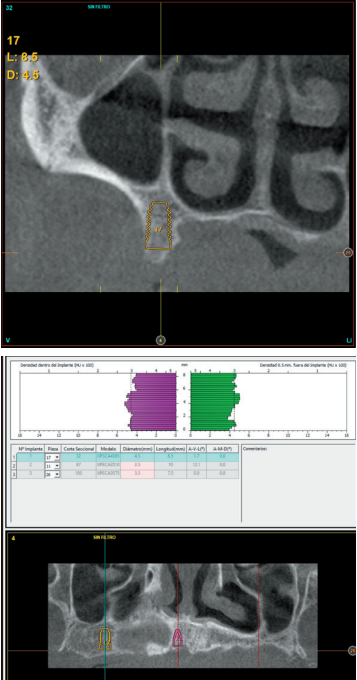
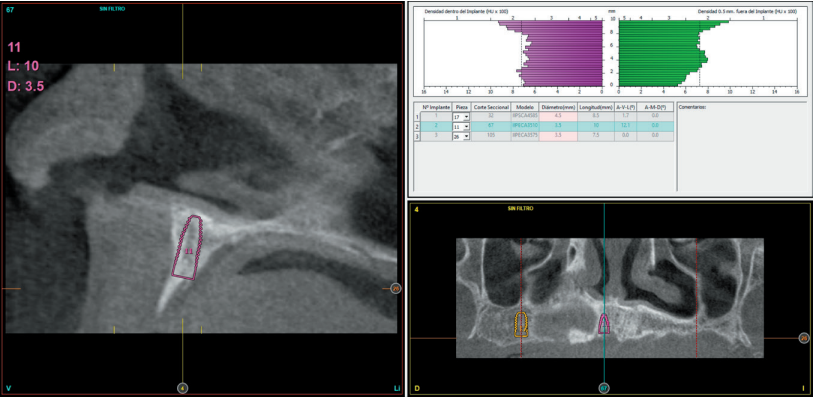
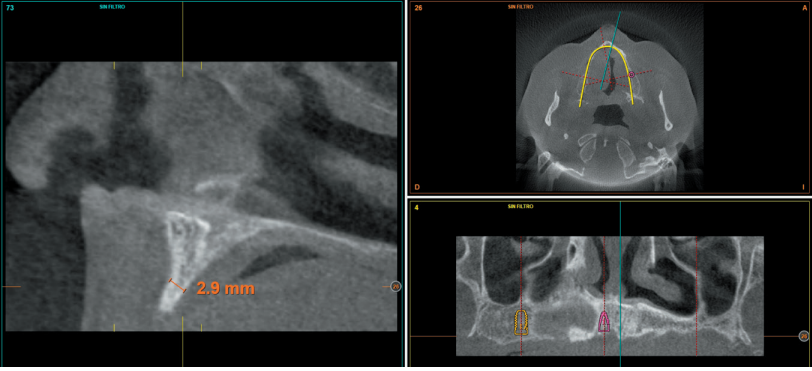
In the areas corresponding to teeth 11 and 13 the horizontal atrophy is even more marked. There is no trabecular bone separating the two corticals (vestibular and palatine) and the width is less than 2mm in some areas which is why block grafts are planned in this area. Short implants are planned in the mandible by direct insertion, and the area corresponding to the mandibular branch will be the donor area for the block grafts.
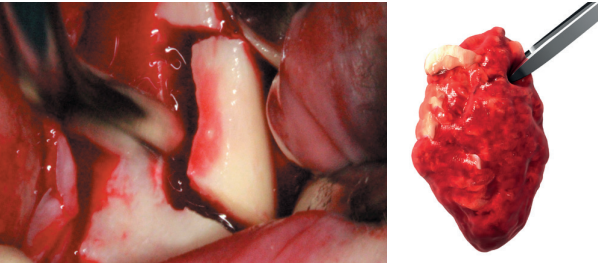
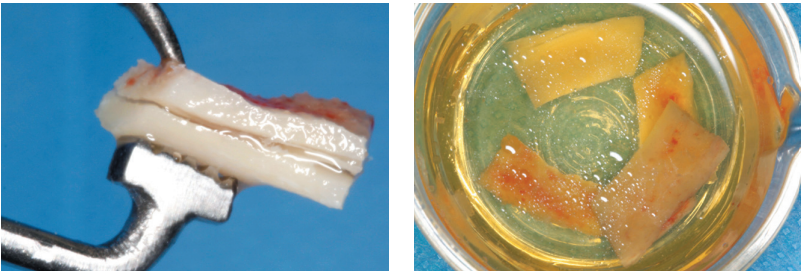
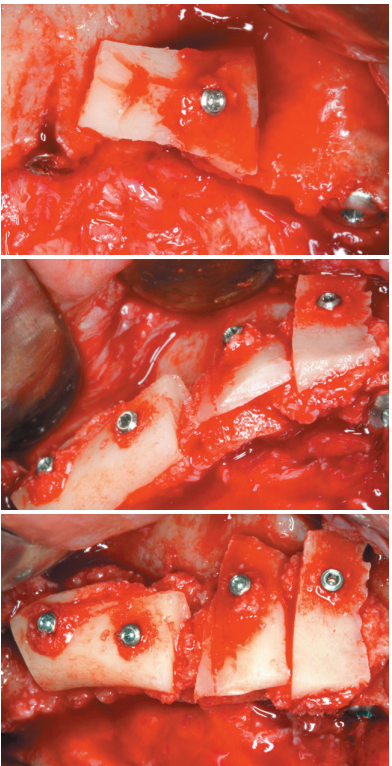
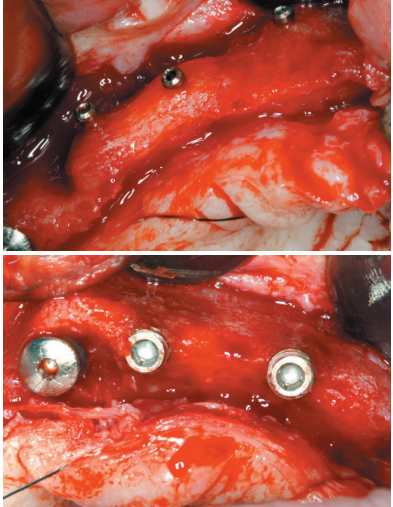
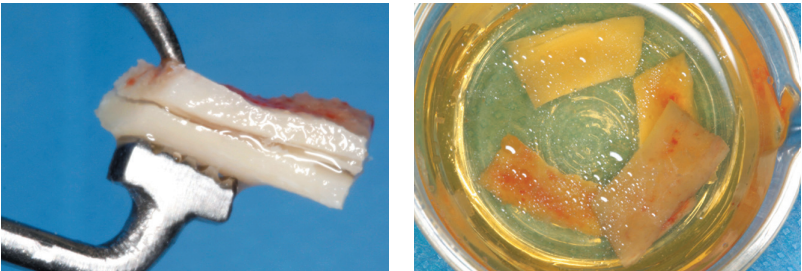
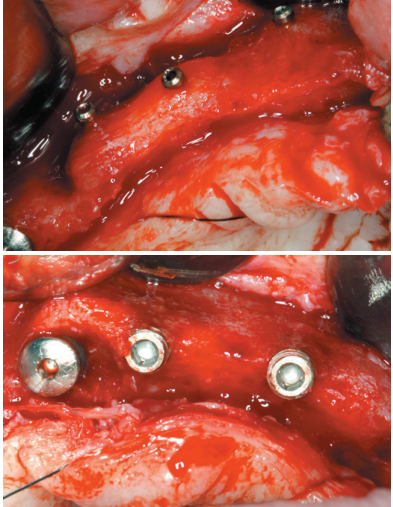
Once the case is planned, the insertion of the lower and upper implants and the different techniques of bone volume increase described is performed. It starts with mandibular surgery to obtain autologous bone obtained from miling that will be preserved during the whole surgery in PRGF-Endoret fraction 2 without activation, to be used in the maxilla where it will be necessary for the grafts in block, according to the technique described by our study group19 (Figures 7 and 8). Once the block graft is obtained it will be divided and maintained in PRGF-Endoret fraction 2 without activation, to maintain its hydration and cell viability until its placement according to the technique described by Khoury where the cortical of the block graft is used as a formwork (Figures 9 and 10)20.
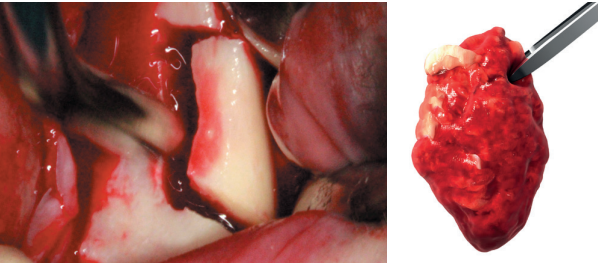
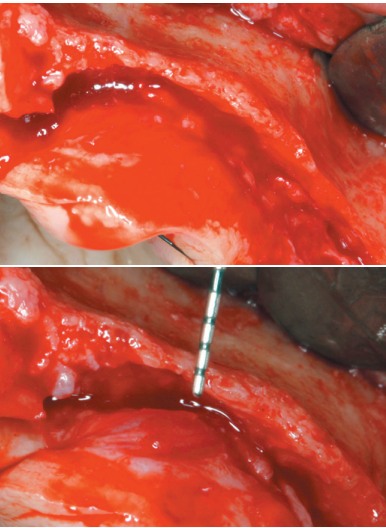
Once the mandibular surgery is finished, the opening of the upper flap is performed, where the great atrophy in horizontal direction that exists in certain locations is noted, as described above, that require performing block grafts (Figures 11 and 12). We proceed to perform the Split technique in two phases (Figure 13) with the insertion of the transitional implants and the insertion of the implants that could be placed directly. Once the insertion of all the implants is completed, the corticals of the grafts are fixed in block, trying to adapt them to the residual morphology as best as possible, avoiding edges that can damage the soft tissue. Once fixed, the gaps are filled mainly with autologous particulated bone obtained from the milling of the lower implants, as well as bone obtained from scraping the mandibular branch (Figures 14-18).
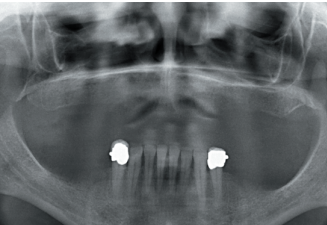
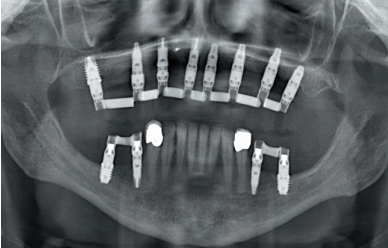
Four months after the initial regeneration of the maxilla surgery a new dental cone-beam is performed, in which the next surgery phase is planned based on the bone gain that has been achieved with the block grafts and the Split technique in two phases. In the images we can see how in the maximum atrophy areas, where the blocks are placed a width has been achieved that triples the initial width (Figures 19 and 20). At the flap opening it is seen as the planification CT images correspond to reality, and also that the area treated by Split in two phases has achieved a crest width that now allows the removal of the transitional implants and the insertion of the new implants in this position, with a better starting and axis situation for the subsequent construction of the prosthesis (Figures 21-22). The implants are inserted and a temporary prosthesis of progressive load is made supported on the implants placed in the first surgical phase. In this way, the patient can have a fixed prosthesis on
implants that will serve to shape the provisional ones in terms of aesthetics and function before the final prosthesis (Figures 23-24).
After four months the loading of the inserted implants in this second surgical phase is carried out. Again, a second provisional prosthesis of progressive loading is chosen, elaborated in the same way as the previous ones. three months aft er the occlusion is prepared for the manufacture of the fi nal prosthesis, so the prosthesis is transformed into a metal-ceramic prosthesis, screwed on transepithelial made by CAD-CAM (Figures 25-26).
The pati ent has recovered the requested functi on, as well as the correction of the occlusion of the complete prosthesis, which presented a right lateral cross bite with decrease in the vertical dimension at the beginning of the treatment. The patient comes to her review and the treatment remains stable as shown in the images taken after 10 years of follow-up (Figures 27-28).
atrophy, we can observe how there is bone volume with less than 2 mm width.

C) Insertion of the transitional implant.
D) Vestibular overcorrection once the transitional implant is inserted.
E) Removal of the transitional implant and new drilling axis.
F) Insertion of the definitive implant.

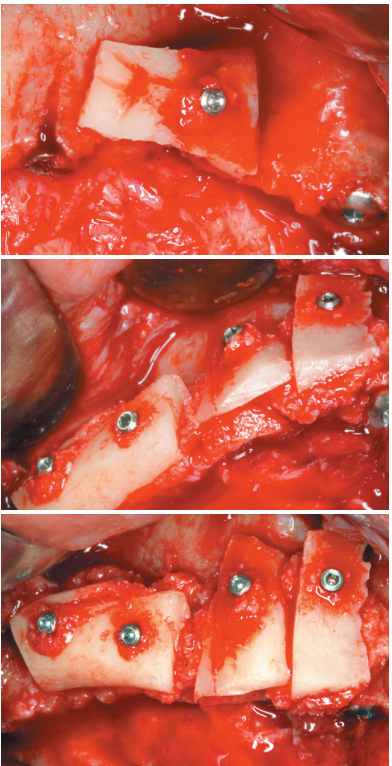
graft and the original autologous bone using bone obtained from drilling embedded in PRGF-Endoret fraction 2. Part of the bone can also be obtained by scraping the mandibular branch with a bone scraper.
crest expansion by transitional implants. The excellent situation for the insertion of the implants is observed.


place.
The regeneration technique of horizontal atrophies with grafts in block and particulate bone as described by Khoury in 200721, presents predictable results in multiple publications in which autologous bone has been used, such as the case that has been studied, as well as with the fusion of autologous bone and biomaterials in cases where the availability of the patient’s bone is not enough20.
The PRGF-Endoret with the particulate bone mixture maintains the viability of the cells until the moment of their use in the block grafting attached to the particle graft technique, and improves the manageability properties of the same, at the same time it increases the ostoinductive potential by increasing the cellular signals contained in the platelet growth factors22-25.
The use of ultrasound to obtain the block graft and the need for a smaller amount of depth of the same, since it will later be divided to be used in different fragments makes the necessary donor block volume smaller and, therefore, the volume of the donor block is lower, so the risk of nerve injury is also minimized by leaving a layer of bone under the extracted graft and separating the donor area of the dental nerve path16.18.
Similarly, the Split technique in two phases, with the use of a transitional expander implant maintains the space of the separation between the vestibular and palatal corticals so that a new bone bridge is formed between both. This increases the width of the residual crest to then be permanently replaced by another implant with the correction of the insertion axis that would give us a conventional Split technique. These advantages have been reported in the technique described by our study group with good results14-26. This type of procedure, in complex cases such as the one addressed in this clinical case, where different surgeries are going to be performed does not increase the morbidity in the patient and guarantees an improvement in the longterm result, by achieving greater bone volume around the definitive implant27,28.
Complex cases require multidisciplinary approaches in which different surgical techniques can be implemented and achieve a successful result. The selection of the correct surgical technique and being able to perform it with the least possible trauma in the patient minimizes the risks of surgery and improves the obtained results.
Kashbour WA, Rousseau NS, Thomason JM, Ellis JS. Provision of information on dental implant treatment: Patients’ thoughts and experiences. Clin Oral Implants Res 2018;29(3):309-19.
Apfel PS. Wisdom. N Y State Dent J
2015;81(5):10-3
Elfadil S, Johnston B, Normand C, Allen F, O’Connell B. An investigation of the characteristics of edentulous patients who choose or refuse implant treatment. Int J Prosthodont 2021;34(2):147–153
Kakudate N, Yokoyama Y, Sumida F,
Matsumoto Y, Riley JL 3rd, Gordan VV, Gilbert GH. Practice-based research agenda priorities selected by patients: findings from a dental practicebased research network. Int Dent J 2019;69(3):183-91.
De Groot RJ, Oomens MAEM, Forouzanfar T, Schulten EAJM. Bone
augmentation followed by implant surgery in the edentulous mandible: A systematic review. J Oral Rehabil 2018;45(4):334-43.
Tolstunov L, Hamrick JFE, Broumand V, Shilo D, Rachmiel A. Bone augmentation techniques for horizontal and vertical alveolar ridge deficiency in oral implantology. Oral Maxillofac Surg Clin North Am 2019;31(2):163-91.
Elnayef B, Porta C, Suárez-López Del
Amo F, Mordini L, Gargallo-Albiol J,
Hernández-Alfaro F. The fate of lateral ridge augmentation: A systematic review and meta-analysis. Int J Oral Maxillofac Implants 2018;33(3):622-35.
Esposito M, Grusovin MG, Felice P,
Karatzopoulos G, Worthington HV, Coulthard P. The efficacy of horizontal and vertical bone augmentation procedures for dental implants – a Cochrane
systematic review. Eur J Oral Implantol 2009;2(3):167-84.
Sanz-Sánchez I, Ortiz-Vigón A, SanzMartín I, Figuero E, Sanz M. Effectiveness of lateral bone augmentation on the
alveolar crest dimension: A systematic review and meta-analysis. J Dent Res 2015;94(9 Suppl):128S-42S
Cortese A, Pantaleo G, Amato M, Claudio PP. Ridge expansion by flapless split crest and immediate implant placement: Evolution of the technique. J Craniofac Surg 2016;27(2):e123-8.
Waechter J, Leite FR, Nascimento
GG, Carmo Filho LC, Faot F. The split crest technique and dental implants: a systematic review and meta-analysis. Int J Oral Maxillofac Surg 2017;46(1):116-28
Anitua E, Begoña L, Orive G. Clinical
evaluation of split-crest technique with ultrasonic bone surgery for narrow ridge expansion: status of soft and hard tissues and implant success. Clin Implant Dent Relat Res 2013;15(2):176-87.
Anitua E, Alkhraisat MH. Is Alveolar
Ridge Split a Risk Factor for Implant Survival? J Oral Maxillofac Surg 2016;74(11):2182-91.
Anitua E, Begoña L, Orive G. Two-stage split-crest technique with ultrasonic bone surgery for controlled ridge expansion: a novel modified technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod
2011;112(6):708-10.
Mendoza-Azpur G, de la Fuente A,
Chavez E, Valdivia E, Khouly I. Horizontal ridge augmentation with guided bone regeneration using particulate xenogenic bone substitutes with or without
autogenous block grafts: A randomized controlled trial. Clin Implant Dent Relat Res 2019;21(4):521-30.
Chappuis V, Cavusoglu Y, Buser D, von Arx T. Lateral ridge Augmentation using autogenous block grafts and guided bone regeneration: A 10-year prospective case series study. Clin Implant Dent Relat Res 2017;19(1):85-96.
Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants 2007; 22 Suppl:49-70. Erratum in: Int J Oral Maxillofac Implants 2008;
23(1):56.
Sánchez-Sánchez J, Pickert FN,
Sánchez-Labrador L, GF Tresguerres
F, Martínez-González JM, Meniz-García C. Horizontal ridge augmentation: A comparison between Khoury and Urban technique. Biology (Basel). 2021 5;10(8):749.
Anitua E, Carda C, Andia I. A novel drilling procedure and subsequent bone autograft preparation: a technical note. Int J Oral Maxillofac Implants. 2007; 22(1):138-45. Erratum in: Int J Oral Maxillofac Implants 2007; 22(2):309.
Khoury F, Hanser T. Mandibular bone
block harvesting from the retromolar
region: a 10-year prospective clinical study. Int J Oral Maxillofac Implants 2015; 30(3):688-97.
Khoury F. Mandibular bone block grafts: Diagnosis, instrumentation, harvesting, technical and surgical procedures. In Khoury F AH, Missika P (ed) Bone Augmentation in Oral Implantology, (ed. Chicago, Quintessence, 2007, p 169).
Solakoglu Ö, Heydecke G, Amiri N, Anitua E. The use of plasma rich in growth factors (PRGF) in guided tissue regeneration and guided bone regeneration. A review of histological, immunohistochemical, histomorphometrical, radiological and clinical results in humans. Ann Anat 2020; 231:151528.
Chou TM, Chang HP, Wang JC.
Autologous platelet concentrates in
maxillofacial regenerative therapy.
Kaohsiung J Med Sci 2020; 36(5):305-10.
Anitua E, Prado R, Orive G. Platelet-rich plasma therapies: Building the path to evidence. J Orthop 2016;14(1):68-9
Anitua E, Sánchez M, Zalduendo MM,
de la Fuente M, Prado R, Orive G, Andía I. Fibroblastic response to treatment with different preparations rich in growth factors. Cell Prolif 2009; 42(2):162-70.
Anitua E, Begoña L, Orive G. Controlled ridge expansion using a two-stage splitcrest technique with ultrasonic bone surgery. Implant Dent 2012;21(3):163-70.
Bare-Welchel B, Campbell PM, Gonzalez M, Buschang PH. Effects of bone grafting, performed with corticotomies and buccal tooth movements, on dehiscence formation in dogs. Am J Orthod Dentofacial Orthop 2017;151(6):1034-47.
Esposito M, Thomsen P, Ericson LE,
Lekholm U. Histopathologic observations on early oral implant failures. Int J Oral Maxillofac Implants 1999;14(6):798-810.

Anitua, Eduardo
Private practice in oral implantology, Eduardo Anitua Clinic, Vitoria, Spain.
University Institute for Regenerative Medicine and Oral Implantology – UIRMI (UPV/ EHU Eduardo Anitua Foundation), Vitoria, Spain.
BTI Biotechnology institute (BTI),
Vitoria, Spain.