Clinical case
Published in spanish Científica Dental Vol. 17. Nº 1. 2020 www.cientificadental.es
Atrophic posterior maxilla: sinus elevation with lateral approach Vs. Extra-short implants. Clinical case with eight years of follow-up
Vertical bone loss in the posterior maxillary sectors is a frequent occurrence after tooth extraction. These areas can often be rehabilitated using regeneration techniques or by opting for a more conservative approach with short implants.
The present clinical case shows bilateral rehabilitation with two different techniques: sinus lift and the insertion of short implants, with a follow-up of 8 years where both techniques have achieved equally predictable results.
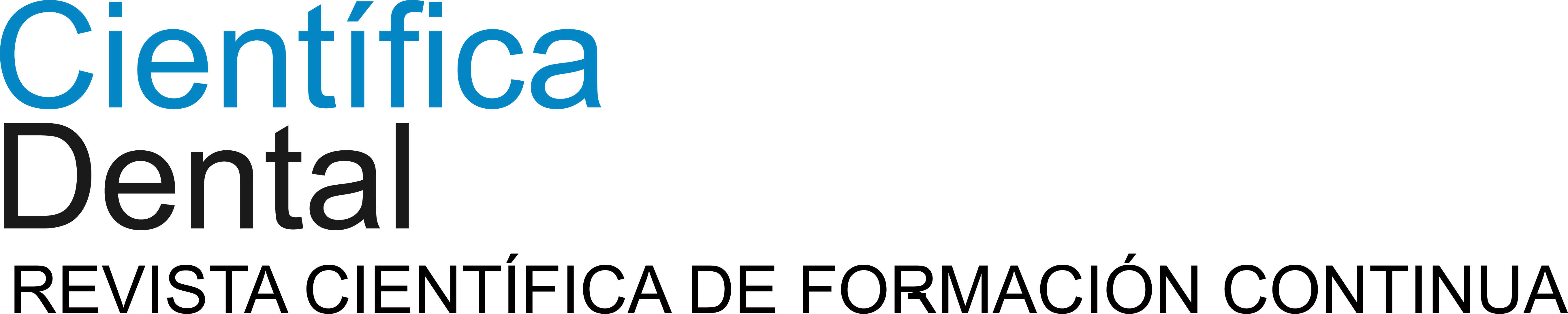
Approaching the posterior sectors of the maxilla with extreme resorption is a common situation in dental practice. The loss of antral teeth produces pneumatisation of the maxillary sinus, which progressively occupies the space corresponding to the dental roots, in some cases leading to complete atrophy and in a residual bone height of 1-2 mm aft er the dental socket heals. This pneumatisation occurs over ti me aft er tooth extraction, but is unpredictable in terms of quanti ty and speed, and appears to be slightly related to the type of relationship that occurs between the apex and the sinus. This relationship was described by Sharan and Madjar in 2008, who established a classification with greater pneumatisation is expected in its types 3 and 4 (Figure 1)1 .

the floor of the maxillary sinus.
Type 0: The root is not in contact with the sinus cortex.
Type 1: The sinus cortex is less convex and makes slight contact with the upper area of the root apex.
Type 3: The sinus cortex describes a curve of lower convexity and the apices of the roots of the antral teeth project into the sinus.
Type 4: The sinus cortex is less concave surrounding the apices
of the antral teeth, and there may be a slight prolongation of the root apices inside the sinus.
Until the arrival of short and extra-short implants, the only alternative treatment in these cases was sinus elevation (laterally or transcrestally), and there were different techniques and procedures for this. The attempt was to gain the lost bone volume and the subsequent insertion of conventional length implants at this level2-6.
The development of short implants and the entire technique for their use sometimes allows the insertion of implants in large posterior vertical atrophies of the maxilla, avoiding sinus elevations.
Nowadays, most authors accept short implants to be those with a length less than 8.5 mm, although there are many cases of lengths well below this figure7-9. Extra-short implants, meanwhile, have more variation in terms of their classification; although the latest articles published consider extra-short implants to be those with a length less than 7 mm10-12. These shorter implants mean less morbidity for pati ents, at the same ti me as it is now possible to rehabilitate pati ents who may refuse to have additional techniques performed. These are sinus elevation and even more complex techniques which may be contraindicated in these pati ents for different medical reasons13-17. These short and extra-short implants can be inserted in the atrophic areas of the maxilla directly without displacement of the lower sinus cortex and without therefore having to manoeuvre the maxillary sinus. The main surgical challenge with this technique is to achieve implant stability, since generally in these cases we are faced with little remaining bone height and with high porosity18-22. Therefore, the establishment of a careful surgical protocol based on drilling into the receptor bed depending on its condition is key to the success of these treatments13-17.
The clinical case described is of a patient receiving both procedures: extra-short implants inserted directly into one maxillary quadrant and a sinus lift with conventional length implants in the other quadrant. The evolution of both treatments in the same patient was able to be observed over eight years.
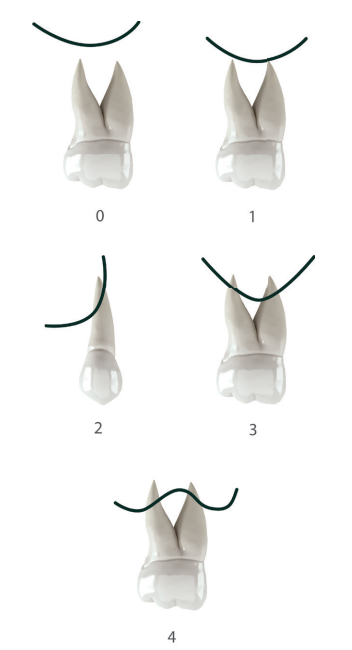
This was the case of a 58-year-old female patient who attended the dentist practice to assess the 16th and 17th molars for pain and mobility. On clinical examination, mobility of both was observed with suppuration at the level of the sulcus. Radiography confirmed our diagnosis of considerable bone loss and sinus perforation at the apex of both molars (Figure 2).
Both teeth were extracted and alveoli regenerated with PRGF-Endoret to seal the perforation and provide the most favourable evolution possible for subsequent insertion of the implants in the area.
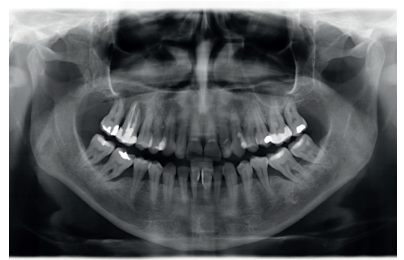
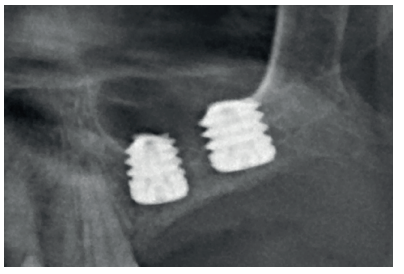
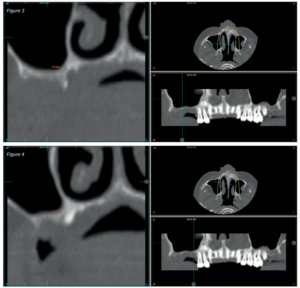
After two months, the dental cone-beam showed the perforation had closed completely but the residual bone volume provided 2 mm of bone height only, which was insufficient to insert the implants (Figures 3 and 4).
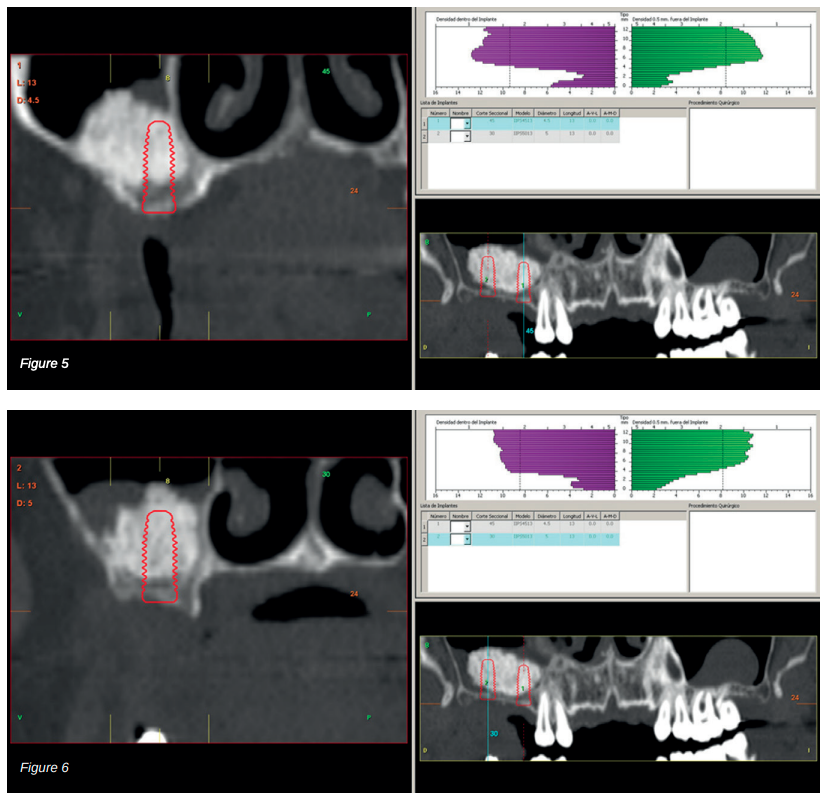
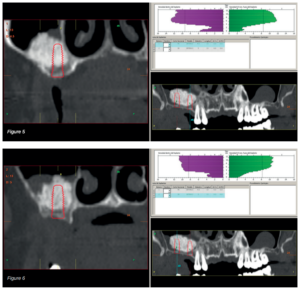
Therefore, it was decided to carry out a sinus lift using biomaterial (bovine hydroxyapatite) bound to PRGFEndoret. The elevation was performed and after five months a new dental cone beam displayed the quantity and quality of the graft obtained for the insertion of dental implants. In the cuts corresponding to the molars of the first quadrant, we observed excellent consolidation of the graft with space to insert 13 mm implants. Today, we would not choose this implant length, since studies published by our group with short and extra-short implants support their use, in addition to showing their diameter is more important than the length to distribute the loads of an already integrated implant; where an 8.5 mm length implant would work in the same way as a 13 mm implant of the same diameter18.
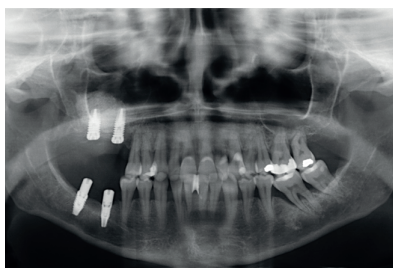
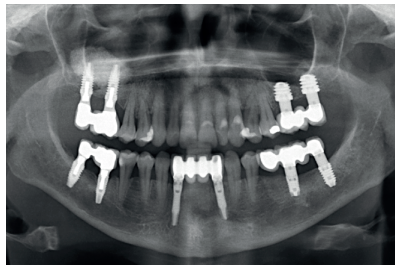
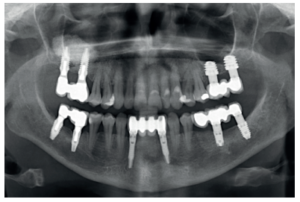
Back in 2007, the therapeutic protocol for these cases was very different (Figures 5-7), with short implants without full development – and without studies demonstrating the importance of diameter over implant length – efforts were focused on the search for anchorage by implant length instead of looking for the bicortical (vestibular-lingual) stability that short and wide implants perform. During this time, the failure of molars 46 and 47 also occurred; these were also extracted and replaced with dental implants.
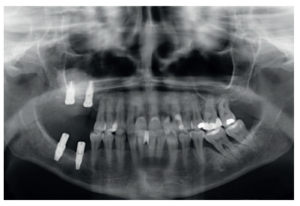
Six months after implant placement, the final prosthesis was made by using a cemented bridge. This prosthetic protocol is also not one we currently use, where tightness, sealing and the use of screw-retained prostheses using an intermediate or transepithelial component prevail. However, at that time, this type of rehabilitation and the conformation of a “bio” emergence profile in the abutments was how these cases were treated (Figure 8)13- 18. The implementation of transepithelial implants in screwretained prostheses opens a new horizon in the prosthesis, changing our working group protocol of towards an improvement in the implant-prosthesis seal, at the same time as prosthetic imbalance is reduced (due to taking the impression directly on the transepithelial and not on the implant connection) and tightness is improved; which reduces the risk of peri-implantitis, among other things19-20.
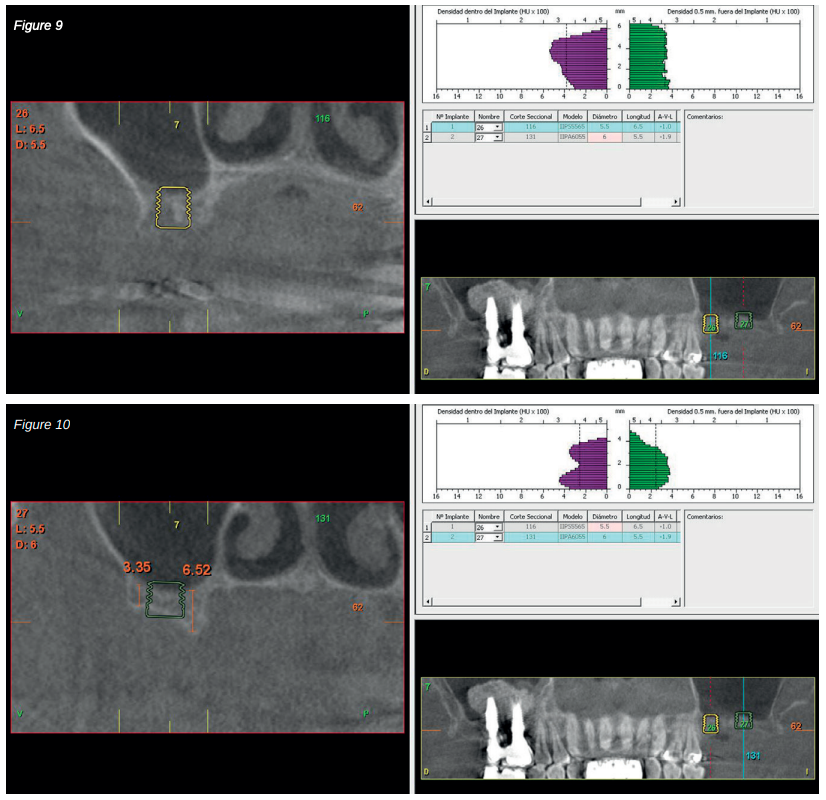
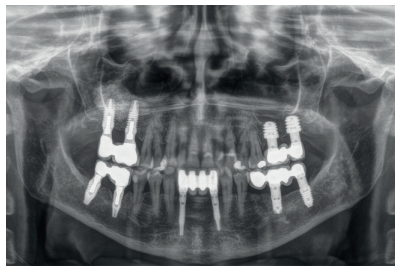
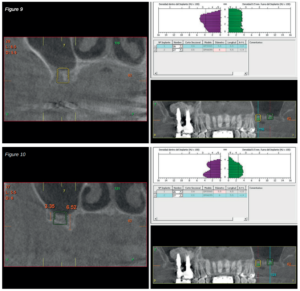
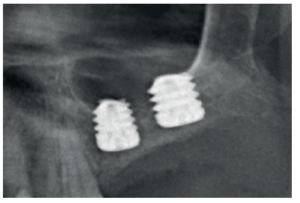
After 4 years, the second and third quadrant molars began to have excessive mobility and serious periodontal problems, so it was decided to remove them and regenerate the alveoli with PRGF-Endoret. Once the area was regenerated (a month and a half later), a conebeam was performed to evaluate the residual bone volume. It can be seen how there was an uneven bone crest with areas of 3.3 mm in height up to a maximum of 7 mm (Figures 9 and 10). On this occasion, due to the protocol change described above, we opted for the direct insertion of extra-short implants, since the surgical protocols to address this type of situation in 2011 varied substantially, with these implants being a first-line tool for the treatment of this type of atrophy (Figure 11). Two extra-short implants were selected (5.5 mm diameter x 6.5 mm length for tooth 26, and 6 mm diameter x 5.5 mm length for tooth 27).
implants.
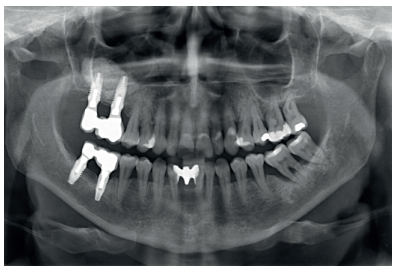
Six months after the insertion of the extra-short implants, the final prosthesis was inserted; in this case, screwed and with an intermediate (transepithelial) component; just as the lower prosthesis in the third quadrant was made. At this point in time, the philosophy of work using a screwretained prosthesis with a transepithelial and the search for tightness and passive fit were the dominant concerns for implant rehabilitation, and this is still so today (Figure 12).
to the one performed in the first quadrant.
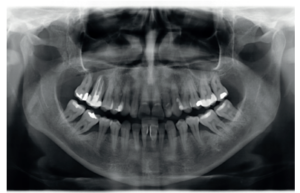
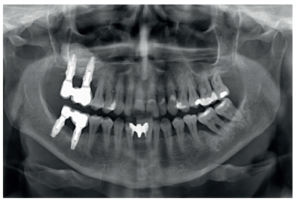
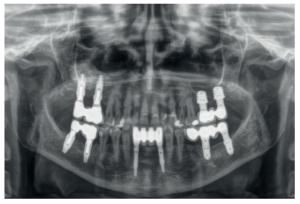
Finally, the stability of both treatments can be seen in the final X-ray at 8 years of age, where both are stable without bone loss (Figure 13).
therapeutic options, with the difference in the morbidity of both
techniques and the times, which have been drastically reduced with the use of short
Therapeutic protocols in implantology have evolved markedly in recent years, moving towards minimally invasive approaches, without renouncing reliability. Therefore, short and extra-short implants are an option used increasingly to avoid aggressive surgeries with high morbidity, and are also an alternative for the rehabilitation of the atrophic posterior maxilla in height, avoiding having to use techniques to lift the sinus when the residual bone height allows15-17.
Since the description of the conventional sinus lifting technique (lateral window) by Tatum in 198622, this procedure has been used for the rehabilitation of posterior maxillary sectors with vertical atrophy, with highly successful rates, currently around 98%, and long-term follow-up (over 15 years)26-27. A drawback of this technique is that it can cause perforation of the Schneiderian membrane and, although today this is no longer an exclusion for the insertion of implants in the same surgery (depending on the extent of the perforation and the case), when this perforation occurs, the success rates of implants inserted in these areas decreases to 88.6%6 . In addition, the need for several surgeries together with a greater increase in patient morbidity, make us opt for less invasive techniques, such as short implants. When inserted in edentulous posterior sectors with elevated vertical resorption, these implants have a lower rate of surgical and prosthetic complications and less marginal bone loss; they are therefore a reliable alternative to bone augmentation procedures and subsequent implant insertion28.
Summers in 1994 described the first variation of the lateral approach technique with a modification to reduce its invasiveness. This technique consists of an approach from the alveolar crest through the use of progressive calibre osteotomes that make a hole that serves both for the elevation of the Schneiderian membrane and the subsequent placement of the dental implant29. This technique has been widely used for the crestal approach of the extreme posterior resorption of the maxilla, with survival figures of the inserted implants between 88.65%30 and 100%31.
Other techniques have been used to approach the atrophic posterior maxilla to varying degrees; such as bone distraction, zygomatic implants, en bloc grafts and guided bone regeneration. All of them have similar success rates to the two shown in this clinical case; with the short and extra-short implants being the ones with the lowest rate of complications and morbidity for the patient32-35.
Long-term survival of short implants also has a very similar rate to that of long implants with sinus lift; therefore, both can be considered as the technique of choice. However, from the point of view of morbidity, the short implants are the better alternative36-37.
In the clinical case described, both therapeutic alternatives show successful treatment for this clinical situation and this specific patient, and can be considered equally valid for resolving the vertical atrophy of the maxilla. For cases with a higher degree of vertical atrophy or those with different bone density and residual volume, the application of one or another technique must be assessed for the success of the treatment.
Sharan A, Madjar D. Maxillary sinus pneumatization following extractions: a radiographic study. Int J Oral Maxillofac Implants 2008; 23(1):48-56.
Correia F, Pozza DH, Gouveia S, Felino A, Faria E, Almeida R. The applications of regenerative medicine in sinus lift procedures: A systematic review. Clin Implant Dent Relat Res 2018; 20:229-242.
Cho YS, Chong D, Yang SM, Kang B. Hydraulic Transcrestal Sinus Lift: Different Patterns of Elevation in Pig Sinuses. Implant Dent 2017; 26:706-10.
Li Y, Hu P, Han Y, Fan J, Dong X, Ren H, Yang C, Shi T, Xia D. Ex vivo comparative study on three sinus lift tools for transcrestal detaching maxillary sinus mucosa. Bioengineered 2017; 4(8):359-66.
Silva LD, de Lima VN, Faverani LP, de Mendonça MR, Okamoto R, Pellizzer EP. Maxillary sinus lift surgery-with or without graft material? A systematic review. Int J Oral Maxillofac Surg 2016; 45:1570-6.
Borgonovo AE, Vitaliano T, Medagliani P, Bianchi A, Re D. Crestal sinus lift by using a mini-invasive procedure: a case series. Minerva Stomatol 2016; 65:107-17.
Esfahrood ZR, Ahmadi L, Karami E, Asghari S. Short dental implants in the posterior maxilla: a review of the literature. J Korean Assoc Oral Maxillofac Surg 2017; 43:70-6.
Lemos CA, Ferro-Alves ML, Okamoto R, Mendonça MR, Pellizzer EP. Short dental implants versus standard dental implants placed in the posterior jaws: A systematic review and meta-analysis. J Dent 2016; 47:8-17.
Cannizzaro G, Felice P, Leone M, Viola P, Esposito M. Early loading of implants in the atrophic posterior maxilla: lateral sinus lift with autogenous bone and Bio-Oss versus crestal mini sinus lift and 8-mm hydroxyapatite-coated implants: a randomised controlled clinical trial. Eur J Oral Implantol 2009; 2:25-38.
Gürlek Ö, Kaval ME, Buduneli N, Nizam N. Extra-short implants in the prosthetic rehabilitation of the posterior maxilla. Aust Dent J 2019; 64:353-8.
Calvo-Guirado JL, Morales-Meléndez H, Pérez-Albacete Martínez C, Morales-Schwarz D, Kolerman R, Fernández-Domínguez M, Gehrke SA, Maté-Sánchez de Val JE. Evaluation of the surrounding ring of two different extra-short implant designs in crestal bone maintanence: A histologic study in dogs. Materials (Basel). 2018 6;11(9) doi: 10.3390/ma11091630.
Pommer B, Mailath-Pokorny G, Haas R, Buseniechner D, Millesi W, Fürhauser R. Extra-short (< 7 mm) and extra-narrow diameter (< 3.5 mm) implants: a meta-analytic literature review. Eur J Oral Implantol 2018;11 Suppl 1: S137-S146.
Anitua E, Alkhraisat MH. 15-year follow-up of short dental implants placed in the partially edentulous patient: Mandible Vs maxilla. Ann Anat 2019; 222:88-93.
Hernández-Marcos G, Hernández-Herrera M, Anitua E. Marginal bone loss around short dental implants restored at implant level and with transmucosal abutment: A retrospective study. Int J Oral Maxillofac Implants 2018; 33:1362-7.
Anitua E, Piñas L, Escuer-Artero V, Fernández RS, Alkhraisat MH. Short dental implants in patients with oral lichen planus: a long-term follow-up. Br J Oral Maxillofac Surg 2018; 56:216-20.
Anitua E. Immediate loading of short implants in posterior maxillae: Case series. Acta Stomatol Croa 2017; 51:157-62.
Anitua E, Flores J, Flores C, Alkhraisat MH. Long-term outcomes of immediate loading of short implants: A controlled retrospective cohort study. Int J Oral Maxillofac Implants 2016; 31:1360-6.
Anitua E, Tapia R, Luzuriaga F, Orive G. Influence of implant length, diameter, and geometry on stress distribution: a finite element analysis. Int J Periodontics Restorative Dent 2010; 30:89-95.
Anitua E. A new approach for treating peri-implantitis: Reversibility of osseointegration. Dent Today 2016; 35:130-1.
Anitua E, Murias-Freijo A, Alkhraisat MH. Conservative implant removal for the analysis of the cause, removal torque, and surface treatment of failed nonmobile dental implants. J Oral Implantol 2016; 42:69-77.
Villarinho EA, Triches DF, Alonso FR, Mezzomo LAM, Teixeira ER, Shinkai RSA. Risk factors for single crowns supported by short (6-mm) implants in the posterior region: A prospective clinical and radiographic study. Clin Implant Dent Relat Res 2017; 19:671-80.
Esfahrood ZR, Ahmadi L, Karami E, Asghari S. Short dental implants in the posterior maxilla: a review of the literature. J Korean Assoc Oral Maxillofac Surg 2017; 43:70-6.
Lemos CA, Ferro-Alves ML, Okamoto R, Mendonça MR, Pellizzer EP. Short dental implants versus standard dental implants placed in the posterior jaws: A systematic review and meta-analysis. J Dent 2016; 47:8-17.
Anitua E, Alkhraisat MH, Piñas L, Orive G. Efficacy of biologically guided implant site preparation to obtain adequate primary implant stability. Ann Anat 2015; 199:9-15.
Tatum H. Maxillary and sinus implant reconstructions. Dent Clin North Am 1986; 30:1207-29.
Beretta M, Poli PP, Grossi GB, Pieroni S, Maiorana C. Long-term survival rate of implants placed in conjunction with 246 sinus floor elevation procedures: results of a 15-year retrospective study. J Dent 2015; 43:78-86.
Viña-Almunia J, Peñarrocha-Diago M, Peñarrocha-Diago M. Influence of perforation of the sinus membrane on the survival rate of implants placed after direct sinus lift. Literature update. Med Oral Patol Oral Cir Bucal 2009;14: E133-6.
Tolentino da Rosa de Souza P, Binhame Albini Martini M, Reis Azevedo-Alanis L. Do short implants have similar survival rates compared to standard implants in posterior single crown?: A systematic review and meta-analysis. Clin Implant Dent Relat Res 2018; 20(5):890-901.
Summers RB. A New Concept in maxillary implant surgery: the osteotome technique. Compendium 1994;15:154–6.
Cavicchia F, Bravi F, Petrelli G. Localized augmentation of the maxillary sinus floor through a coronal approach for the placement of implants. Int J Periodontics Restorative Dent 2001; 21:475-85.
Del Fabbro M, Corbella S, Weinstein T, Ceresoli V, Taschieri S. Implant survival rates after osteotome-mediated maxillary sinus augmentation: a systematic review. Clin Implant Dent Relat Res 2012; 14(Suppl 1): e159-68.
Petrungaro PS, Kurtzman GM, Gonzales S, Villegas C. Zygomatic implants for the management of severe alveolar atrophy in the partial or completely edentulous maxilla. Compend Contin Educ Dent 2018; 39:636-45.
Faot F, Thomé G, Bielemann AM, Hermann C, Melo AC, Padovan LE, de Mattias Sartori IA. Simplifying the treatment of bone atrophy in the posterior regions: Combination of zygomatic and wide-short implants-a case report with 2 years of follow-up. Case Rep Dent 2016; 2016:5328598.
Bastos AS, Spin-Neto R, Conte-Neto N, Galina K, Boeck-Neto RJ, Marcantonio C, Marcantonio E, Marcantonio E Jr. Calvarial autogenous bone graft for maxillary ridge and sinus reconstruction for rehabilitation with dental implants. J Oral Implantol 2014; 40:469-78.
Pistilli R, Signorini L, Pisacane A, Lizio G, Felice P. Case of severe bone atrophy of the posterior maxilla rehabilitated with blocks of equine origin bone: histological results. Implant Dent 2013; 22: 8-15.
Gastaldi G, Felice P, Pistilli R, Barausse C, Trullenque-Eriksson A, Esposito M. Short implants as an alternative to crestal sinus lift: a 3-year multicentre randomised controlled trial. Eur J Oral Implantol 2017; 10:391-400.
D’Amato S, Borriello C, Tartaro G, Itro A. Maxillary sinus surgical lift. Summers’ technique versus lateral surgical approach. Minerva Stomatol 2000; 49:369-81.

Anitua, Eduardo
Doctor in medicine. Private practice in Oral Implantology. Eduardo Anitua Clinic, Vitoria. University Institute for Regenerative Medicine and Oral Implantology – UIRMI (UPV / EHU Fundación Eduardo Anitua), Vitoria. 3 BTI Biotechnology Institute, Vitoria.