Clinical case
Published in spanish Científica Dental Vol. 20. Nº 2. 2023
Implant explantation poorly positioned in an aesthetic sector and subsequent regeneration with block grafting. Clinical case
Performing an explantation in the aesthetic sector produces a defect that often leaves a bone loss that must be regenerated through different procedures. Bone block grafting can be an alternative in cases where simultaneous vertical and horizontal bone regeneration is required. In this clinical case we show the explantation of a poorly positioned implant in the aesthetic sector, impossible to rehabilitate, which must be explanted and the defect subsequently regenerated so that a new implant can be positioned, this time in a situation that allows us a predictable and aesthetically satisfactory rehabilitation.
Replacement with an immediate post-extraction implant is a very common technique for teeth located on the aesthetic front, especially the maxilla. In many cases, in order to stabilise these implants, the aim is to increase their length (apical anchorage) and the morphology or the previous defect left by the alveolus sometimes forces us to an excessive over-angulation of the implant or a too vestibularised placement, with the subsequent difficulty of an adequate prosthetic rehabilitation1,2. Therefore, to perform a correct planning of each of the cases in this area it should be carried out leaving for a later phase (either completely postponed after healing or during early bone healing) the placement of the implant, allowing us to correct some of these errors1-3.
When a patient presents an implant located in the aesthetic sector with infectious problems or incorrect placement, which prevents its correct rehabilitation, the treatment plan is complicated, since the case must be started again, but in both hard and soft tissue with worse conditions that at the beginning of the treatment4. Therefore, having a technique that allows removing the implant with the least possible bone loss in the area is ideal, since this ensures a better starting situation for the new implant regeneration and rehabilitation6. The used atraumatic explantation kit (KEXIM- Biotechnology Institute®)5-8 ensures the removal of the implant without damaging the bone tissue in which it is located, in a quick and simple way, being able to subsequently insert a new implant in the same area and surgical procedure in those cases where it is indicated.
In this clinical case, there is an implant placed in an erroneous position in the anterior sector, in an area where the rehabilitation space is seriously compromised (lateral incisor zone), and where one must be as conservative as possible in the explantation to have a better chance. In the development of the case, the planning performed for its explantation, regeneration and subsequent insertion of a new implant is shown, along with its prosthetic rehabilitation and the follow-up of the case over time to verify that the stability of the treatment performed is maintained.
We present the case of a 36-year-old woman who comes to the clinic demanding solution for an implant located in position 1.2. This implant has carried a rehabilitation with a crown for a short period of time in which an important mucositis and loss of the thickness of the gingival tissue occurred, for which the crown was removed. The patient has a provisional removable crown and the soft tissue surrounding the area of the initial emergency of the implant-supported prosthesis is in bad condition, with a significant loss of thickness and the remains of a soft tissue fistula (Figures 1-4).
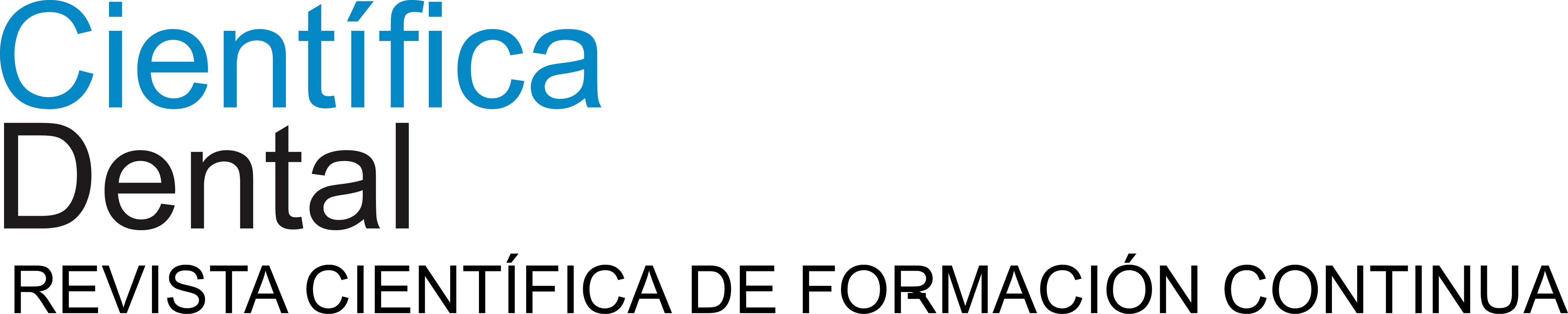
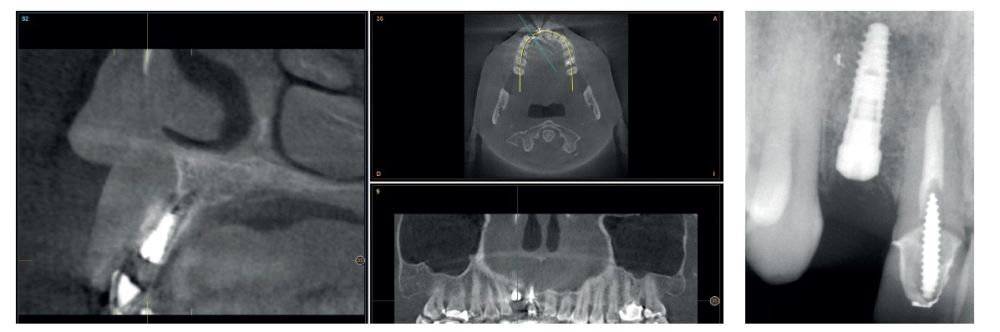
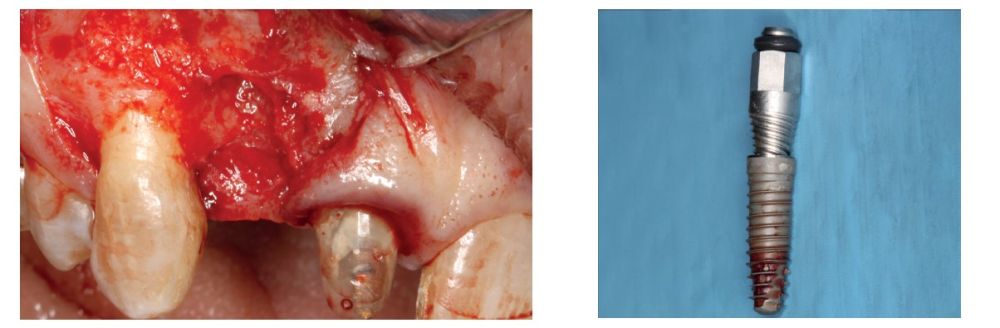
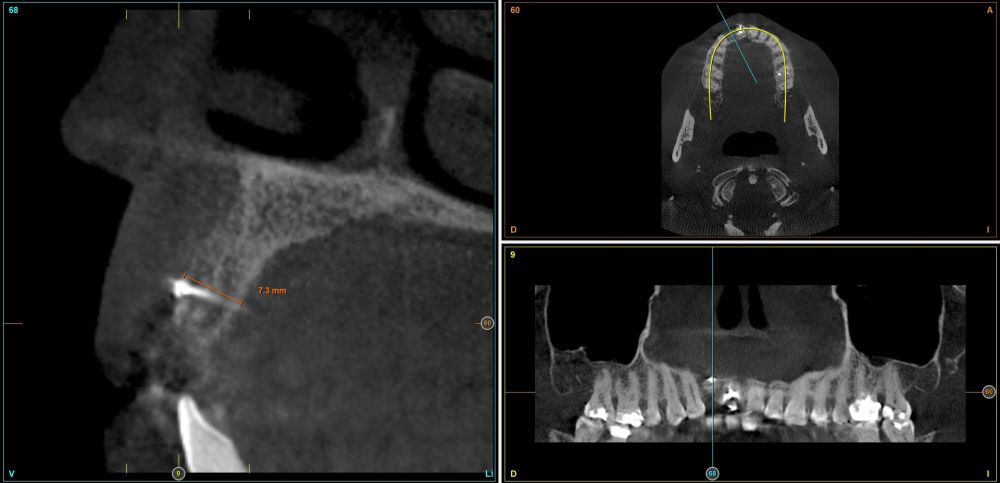
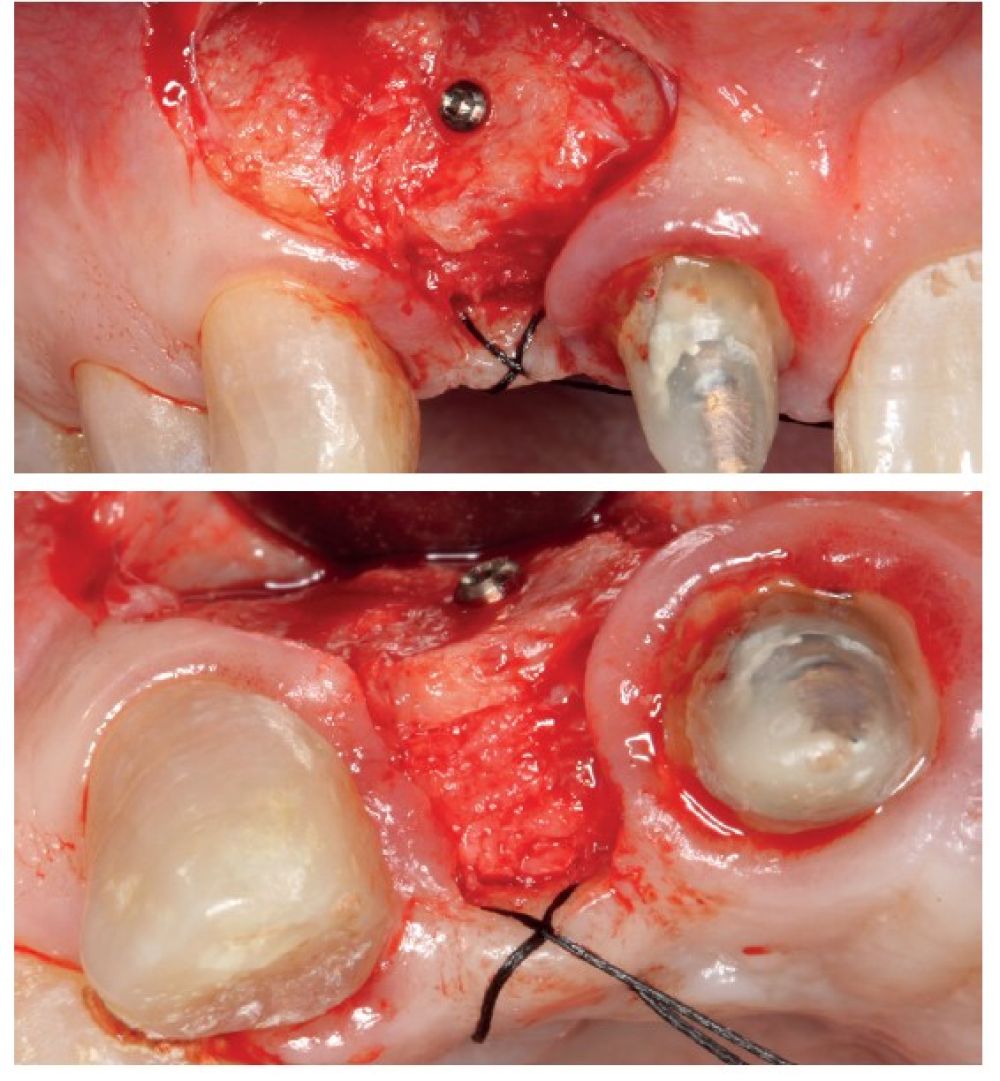
To continue with the study of the case, a Cone Beam is performed where we can observe three-dimensionally the position of the implant located in position 1.2. In the sectional cuts it is visualized completely positioned toward vestibular with an almost complete resorption of the cortical bone of this area, which explains the underlying soft tissue problems. The periapical radiography shows the position of the implant with respect to adjacent teeth (Figures 5 and 6). With this image we proceed to create a flap and the explantation of the implant. The crown located in tooth 1.1 is also removed to be able to make another crown that will serve to support the provisional extension for zone 1.2, while the first procedure heals. In this first approach a block grafting obtained from the mandibular ramus is also placed which is fixed with a microscrew in the area to be regenerated where the vestibular cortical has been lost. Once fixed and positioned, it is filled around the block grafting with particulate bone obtained with a bone-scraper of the same donor zone embedded in PRGF-Endoret for better fixation and cellular viability (Figures 7-9).
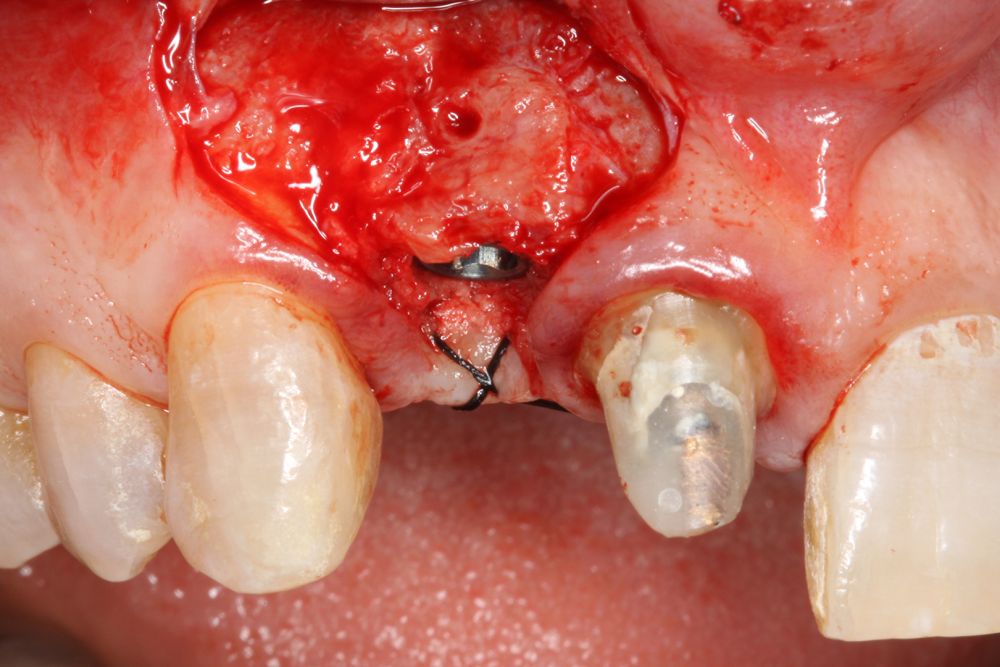
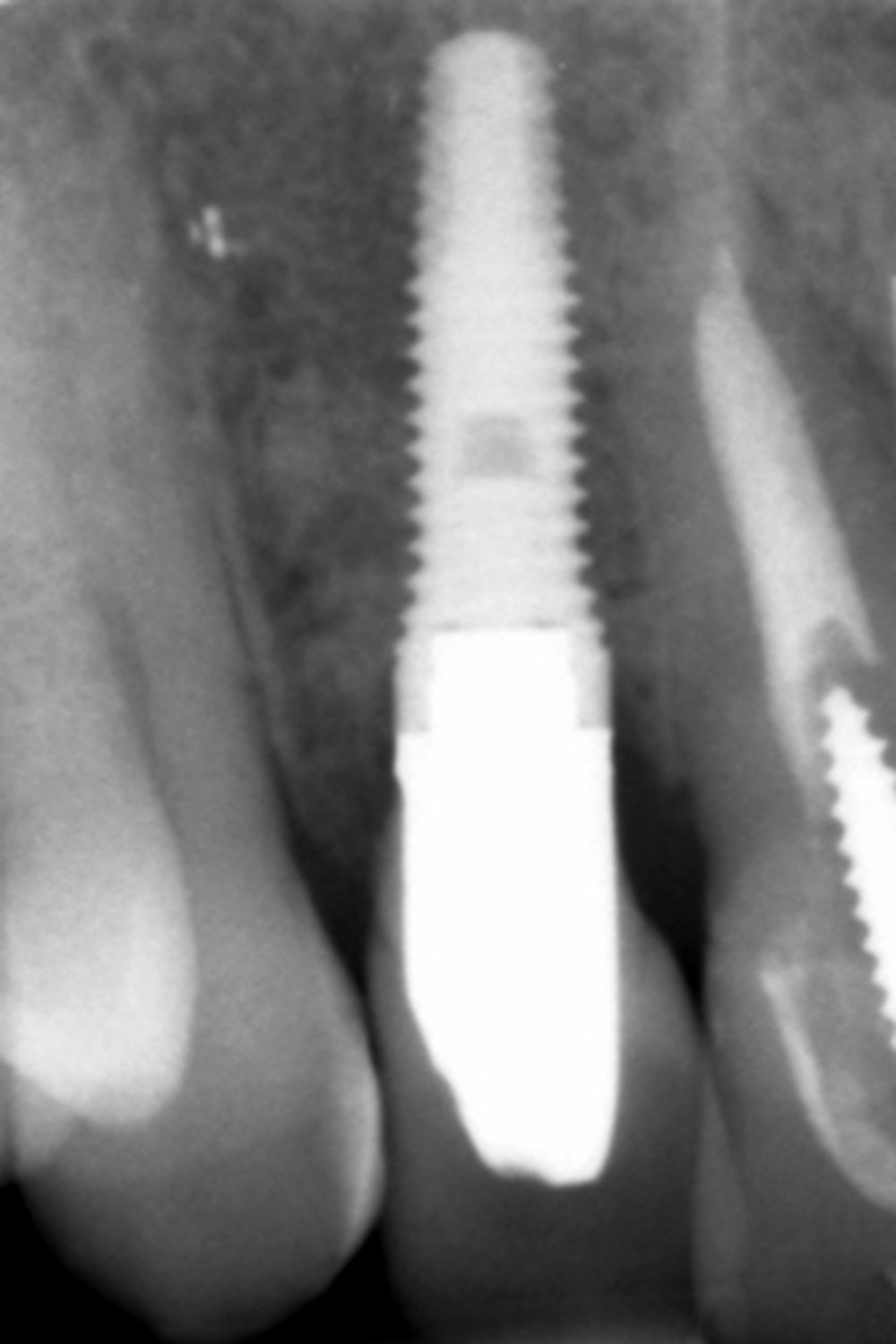
Four months later, a new dental cone-beam is performed to quantify the gain obtained in width with the regenerative procedure. It is observed in the sectional cut that a crest width of more than 7 mm and a complete regeneration of the alveolar ridge has been achieved, allowing the insertion of a new dental implant in the adequate position (Figure 10). In the surgical reentry, the information of the Cone-Beam is verified with a total integration of the graft material, as shown in the clinical images at the time of lifting the flap for the insertion of the implant (Figures 11 and 12). The microscrew is removed and the implant is placed, which is performed by vestibular compression of the graft to gain in this manner even more contour in this area (Figure 13). The implant is left in a surgical phase, with a low healing abutment that allows a subsequent location of the same without an aggressive soft tissue surgery when the construction of the prosthesis is initiated. The provisional crown remains as an extension from the tooth 1.1.
Three months later, the prosthetic phase begins. The state of the gingival tissue is correct, although at vestibular level we would like to achieve a decrease of the zenith of the future tooth, so a connective tissue graft is planned that allows this more appropriate emergence profile conformation. The case ends with E-max crowns at the level of 1.2 and 1.1, achieving a harmonious smile and fully integrated in the rest of the smile, regarding colour, emergence and disposition of the gingival margins (Figures 14-15). The patient continues a follow up for years, maintaining the stability of the performed rehabilitation (Figure 16).
Advanced perimplantitis explantation or removal of implants that are incorrectly positioned and which prosthetic rehabilitation is not possible, complying with functional or aesthetic criteria, is a problem that we have to face in our consultations and for which tools are needed to facilitate the approach. Within the techniques for dental implants removal, there are different procedures, being those based on counter-torque that have proved to be more simple, reliable and conservative with the bone tissue, key to later rehabilitate the area with new dental implants5-10.
The concept of being able to perform an osseodisintegration by counter-torque was introduced by different authors in the 90s, performing experiments in which different implant surfaces were tested and their ability to achieve a better osseointegration with the counter-torque removal of the implants, based on the fact that a better surface area would give higher removal values (implant removal would be more expensive)11-16. Later, this idea is taken up in different tests, among them, those developed by our study group to design in an animal model an explantation kit based on counter-torque that is effective to remove different types of implants with different morphologies and surfaces, in the least traumatic possible manner7.
In the case of incorrect positioned implants, sometimes this defect is due to an initial bone deficit that has caused the position of the implant to be conditioned by the residual bone volume. On other occasions, a greater defect has been generated in the bone than originally existed when the implant technique was performed incorrectly, resulting in a resorption of the alveolar bone17.18, this resorption frequently affects the vestibular cortical, as in the present case. On numerous occasions it is necessary to rebuild the alveolar ridge in order to generate sufficient volume that allows the insertion of the implant safely and with a suitable position for its rehabilitation. When there is a total or partial loss of the vestibular cortical bone one of the most used techniques for regeneration of the area is usually a block graft19. With this procedure we can regenerate the width and height of the defect creating a new absent cortical, thus completely restoring the lost bone architecture.
In cases like the one shown, of a single implant, an additional expansion can also be generated with the implant itself to correct the present defect. The insertion of the implant with expansion gives us an extra correction that makes it gain even more volume at this level. This technique of vestibular expansion of the graft once integrated, through the preparation of the alveolus in a way that generates compression, has been described by our study group with good stable and lasting results over time20. In this case, this procedure has also been used restoring the contour in such an aesthetically important area as the lateral incisor.
Implants that are incorrectly positioned in the aesthetic sector can be extracted in an atraumatic way and reshape the bone tissue that allows the insertion of a new implant in the correct position from the point of view of the posterior prosthetic rehabilitation. For this, atraumatic extractors and different regeneration techniques can be used depending on the bone defect to be restored.
Buser D, Chappuis V, Belser UC, Chen S. Implant placement post extraction in esthetic single tooth sites: when immediate, when early, when late? Periodontol 2000. 2017;73:84-102.
Mao Z, Lee CT, He SM et al. Buccal bone dimensional changes at immediate implant sites in the maxillary esthetic zone within a 4-12-month follow-up period: A systematic review and meta- analysis. Clin Implant Dent Relat Res 2021;23:883-903.
Slagter KW, den Hartog L, Bakker NA, Vissink A, Meijer HJ, Raghoebar GM. Immediate placement of dental implants in the esthetic zone: a systematic review and pooled analysis. J Periodontol. 2014;85:e241-50.
Santos PL, Gulinelli JL, Telles Cda S et al. Bone substitutes for periimplant defects of postextraction implants. Int J Biomater 2013;2013:307136.
Anitua E, Fernandez-de-Retana S, Alkhraisat MH. Performance of the counter-torque technique in the explantation of nonmobile dental implants. Int J Implant Dent 2020;9:6:1.
Winnen RG, Kniha K, Modabber A et al. Reversal of Osseointegration as a Novel Perspective for the Removal of Failed Dental Implants: A Review of Five Patented Methods. Materials (Basel) 2021;17;14:7829.
Anitua E, Murias-Freijo A, Piñas L, Tejero R, Prado R, Orive G. Nontraumatic Implant Explantation: A Biomechanical and Biological Analysis in Sheep Tibia. J Oral Implantol 2016;42:3-11.
Anitua E, Orive G. A new approach for atraumatic implant explantation and immediate implant installation. Oral Surg Oral Med Oral Pathol Oral Radiol 2012;113:e19-25.
Roy M, Loutan L, Garavaglia G, Hashim D. Removal of osseointegrated dental implants: a systematic review of explantation techniques. Clin Oral Investig 2020;24:47-60.
Stajčić Z, Stojčev Stajčić LJ postextraction et al. Removal of dental implants: review of five different techniques. Int J Oral Maxillofac Surg 2016;45:641-8.
Chrcanovic BR, Albrektsson T, Wennerberg A. Reasons for failures of oral implants. J Oral Rehabil 2014;41:443-76.
Wennerberg A, Ektessabi A, Albrektsson T, Johansson C, Andresson B A. A 1-year follow- up of implants of differing surface roughness placed in rabbit bone. Int J Oral Maxillofac Implants 1997; 12:
486-494.
Wennerberg A, Hallgren C, Johansson C, Danelli SA. A histomorphometric evaluation of screw-shaped implants each prepared with two surface roughnesses. Clin Oral Implants Res 1998;9: 11-19.
Trisi P, Rao W, Rebaudi A. A histomorphometric comparison of smooth and rough titanium implants in human low-density jaw bone. Int J of Oral and Maxillofac Impl 1999;14: 58-67.
Johansson C, Albrektsson T. Integration of screw implants in the rabbit.A 1-year follow-up of removal torque of titanium implants. Int J Oral Maxillofac Impl 1987; 2:69 75.
Sennerby L, Thomsen P, Ericsson L.A. Morphometric and biomechanic comparison of titanium implants inserted in rabbit cortical and cancellous bone. Int J Oral Maxillofac Impl 1992: 7: 62-71.
Chen ST, Buser D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla – a systematic review. Int J Oral Maxillofac Implants. 2014;29 Suppl:186-215.
Chen ST, Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants. 2009;24 Suppl:186-217.
Milinkovic I, Cordaro L. Are there specific indications for the different alveolar bone augmentation procedures for implant placement? A systematic review. Int J Oral Maxillofac Surg. 2014;43:606-25.
Anitua E, Murias-Freijo A, Alkhraisat MH. Implant site under-preparation to compensate the remodeling of an rutologous bone blockg. J Craniofac Surg 2015;26:e374-7.

Anitua, E
DDS, MD, PhD. Private practice in oral implantology, Eduardo Anitua Clinic, Vitoria, Spain. Instituto
Universitario para la medicina oral regenerativa e implantología – (University Institute for Regenerative Medicine and Oral Implantology – UIRMI) (UPV/ EHU Eduardo Anitua Foundation), Vitoria, Spain. BTI Biotechnology institute (BTI), Vitoria, Spain.