Systematic review
Published in spanish Científica Dental Vol. 18. Nº 2. 2021 www.cientificadental.es
Use of particulate dentin in alveolar preservation procedures: a systematic review
Introduction: The biological processes that take place following dental extractions cause defects in the soft and hard tissues of the jaw, which hinder rehabilitation techniques with implants. Alveolar preservation procedures have been proposed to decrease these dimensional changes. Although autogenous bone is considered the material with the best properties, it also leads to an increase in patient morbidity. Therefore, the tooth itself is considered as an alternative. The objectives of this review were to analyse the dimensional changes in alveolar ridge height/width after alveolar preservation procedures using particulate dentin, as well as possible intraoperative and postoperative complications, new bone formation and re-entry time in the grafted area.
Materials and method: A review of the relevant literature in the PubMed and MEDLINE databases was carried out, identifying studies evaluating alveolar preservation procedures with particulate dentin in human patients with recorded follow-up.
Results: A total of 12 studies were included in the systematic analysis. The dimensional changes, after grafting with particulate dentin, were comparable to those of other biomaterials and fewer than in the control groups. The occurrence of complications was low. New bone formation and re-entry time were similar to other biomaterials.
Maxillary bones are delicate structures subject to reabsorption processes, which can cause defects and limit implantological rehabilitating techniques1 . Dental extraction is one of the main reasons for these alterations in hard and soft tissue, as it can drastically modify alveolar crest volume2 . Much research has been done to evaluate the effectiveness of various biomaterials in alveolar preservation procedures. Studies in animals3 and humans4 show minor volumetric changes, despite the techniques used to prevent them. Among the biomaterials used in alveolar preservation, autogenous bone is the most predictable due to its rapid revascularisation and resistance to infection5 . However, this biomaterial also has disadvantages, such as limited availability, an increase in morbidity in the process of obtaining it and associated risks during surgery. Particulate dentin, however, is considered as an autogenous alternative with less morbidity. The results reported in the literature on this graft have been satisfactory, in vitro6 , in preclinical models in animals5,7,8 and in clinical studies in humans9,10. The objective of this review was to look at existing evidence about alveolar preservation procedures with particulate dentin.
Protocol
This review was carried out based on the PRISMA criteria (Preferred Reporting Items for Systematic Reviews and Meta-Analyses). A protocol was designed following the PICO system to answer the following question: “In patients awaiting alveolar preservation after tooth extraction, how effective is particulate dentin compared to other grafts or control patients left to heal conventionally?”
(P) Population: Patients who need a tooth extraction
(I) Intervention: Alveolar preservation procedures with particulate dentin
(C) Comparison: Control patients or use of different biomaterials
(O) Outcomes: Dimensional changes in height/ width (mm) of the alveolar crest after the therapy; analysis of intra and postoperative complications; new bone formation; and reentry time.
Search strategy
The search was carried out in April 2020 according to the established inclusion and exclusion criteria, without restrictions for age, gender or race. Included studies were identified using the search terms “(particulate dentin) OR (demineralised dentin matrix) OR (extracted tooth AND ridge preservation) OR (autogenous tooth AND bone graft) OR (extracted tooth AND regeneration)” via PubMed at the MEDLINE database.
Inclusion and exclusion criteria
Inclusion criteria:
- Clinical trials, cross -sectional studies, cases series, case reports, cases control studies and cohort studies.
- Studies that include volumetric changes, complications and/or new bone formation in alveolar preservation procedures with particulate dentin.
- Studies that include patient monitoring.
Exclusion criteria:
- Duplicate studies.
- Studies with no design details.
- In vitro studies in animals, bibliographic reviews, systematic reviews and meta-analyses.
- Studies that included patients with compromised systemic health.
- Studies published in languages other than English or Spanish.
Data organisation
The data obtained from reading the complete manuscripts were collated and organised in two tables as follows:
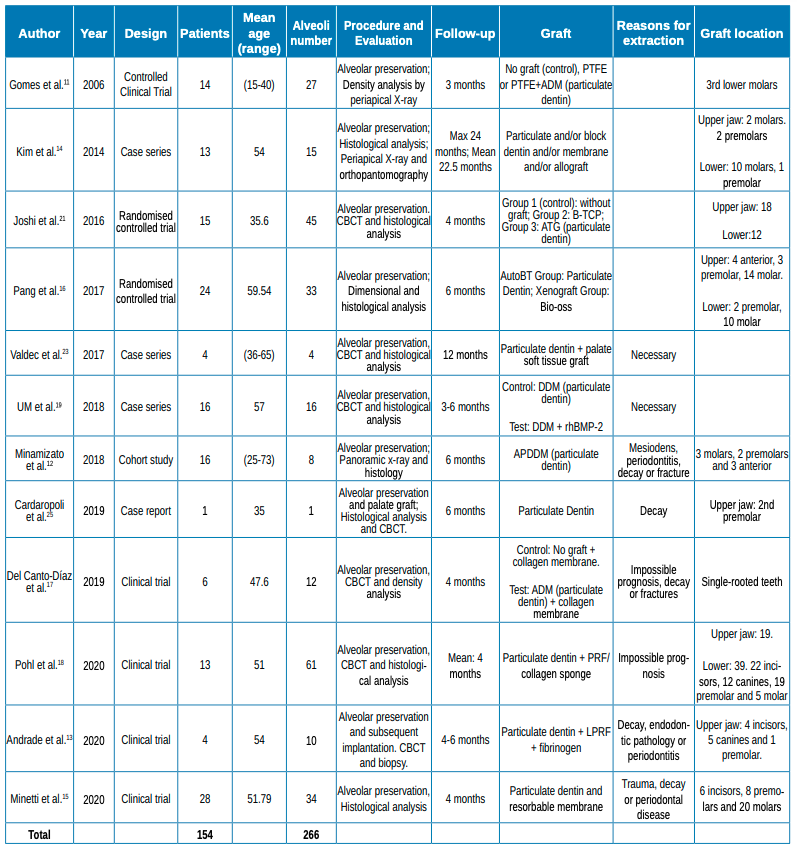
Table 1: Author, study year, study design, number of patients, mean age/age range, number of alveoli, procedure and evaluation, monitoring, graft used, reason for extraction; and graft location.

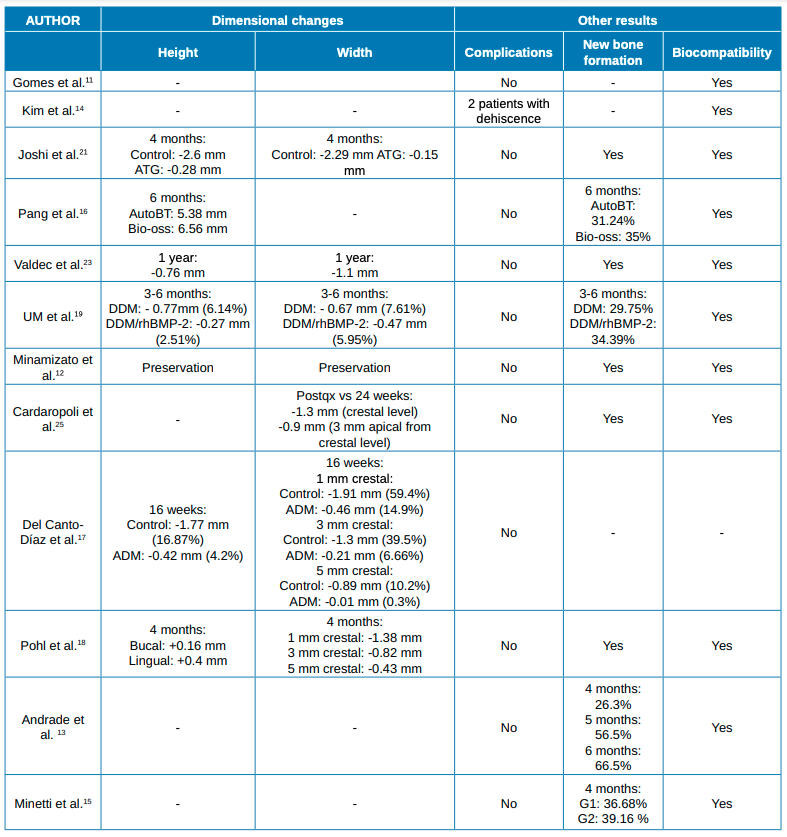
Table 2: Author, height dimension change, width dimension change, complications, new bone formation and re-entry time.

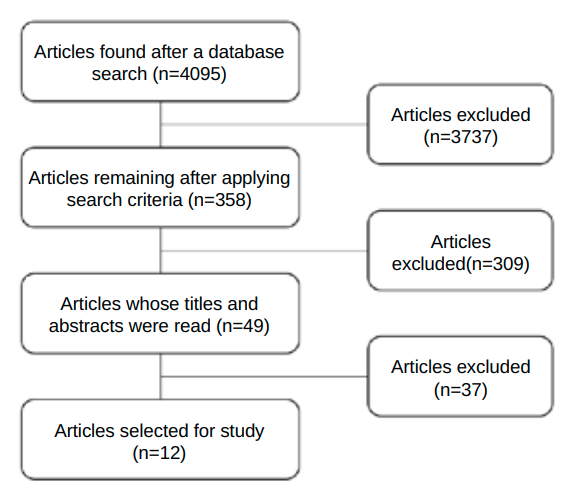
The information flow diagram is shown in Figure 1. The initial search identified a total of 4,095 articles. After applying the search criteria, 3,737 articles were discarded. After reading titles and abstracts, 309 articles were excluded. The complete manuscripts of the remaining 49 articles were read and another 37 were excluded according to the inclusion and exclusion criteria. Finally, 12 articles were included in the review.
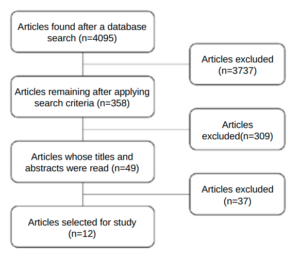
Table 1 contains information from the studies included in the review. Of the articles included (n=12), there were 6 clinical trials, 1 cohort study, 1 case report, 3 case series and 1 retrospective radiographic study. All articles were published between 2006 and 2020. The average age of the patients was between 35 and 59 years, except for 2 studies11,12 that reported ranges between 15 and 73 years. The total number of patients included in the publications selected was 154, which was an average of 12.83 patients per study. The number of alveoli studied was 266, an average of 1.7 per patient. The samples were balanced regarding participant sex.
All studies evaluated the effectiven ess of particulate dentin in alveolar preservation. Some studies also evaluated other regenerative or rehabilitative procedures. Follow-up was between 3 and 24 months. The graft material used was particulate dentin in all studies, combined in some studies with other filler or membrane biomaterials.
Dimensional changes
The dimensional change results are found in Table 2. Except for 4 studies11,13-15, most evaluated the dimensional changes in height and/or width. They were calculated as the difference between the beginning and end of the procedure, except for Pang et al16, who analysed the vertical gain from the end of the defect to a resin model placed on adjacent teeth. Minamizato et al.12 assessed alveolar preservation, but did not quantify it.
Complications
The results for complications are in Table 2. All studies reported an absence of complications in alveolar preservation procedures with particulate dentin, except for one4 , in which two patients developed dehiscence during healing; a second attempt provided proper healing.
New bone formation
The new bone formation results are in Table 2. This was recorded in all but 3 studies11,14,17. All these studies found new bone formation, with the range varying from 26.3% to 66.5%, depending on the study.
Re-entry time
Re-entry time results are in Table 2. This was recorded in all but 3 studies11,17,18, with the rest of the studies recording re-entry time for the insertion of implants and/or taking a biopsy. This period varied between 3 and 6 months.
At present, scientific evidence on the use of particulate dentin in alveolar preservation procedures is limited. Few published studies were identified, and these were of low sample size and short-term follow -up. However, this biomaterial is considered a promising alternative. The purpose of this review was to gather the data reported in the literature evaluating four aspects: (a) vertical and horizontal dimensional changes; (b) intra and postoperative complications; (c) new bone formation; and (d) re-entry time in the grafted area.
Dimensional changes
Vertical:
At 3 and 6 months of the Alveolar preservation, Um et al.19 recorded losses of -0.77 mm (6.14%) in the particulate dentin group. These are similar to losses reported at 6 months by Pelegrine et al.20, who performed alveolar preservation with an autogenous bone graft (0.62 mm).
At 4 months, Joshi et al.21 and Del Canto-Díaz et al.17 analysed losses of -0.28mm and -0.42mm, respectively, in the particulate dentin group. In this same period, Matchei et al.22 reported losses of -0.25 mm in patients grafted with bovine xenograft. These losses were greater at -1.71 mm in the control group of this same study, which left the socket to heal spontaneously.
At 12 months, Valdec et al.23 recorded a loss of -0.76 mm in the particulate dentin group, although at this time the implants had already been placed. However, these results are similar to other studies in the literature, such as Barone et al.24, who recorded -0.7 mm after the use of xenograft. Buccal losses were 3.6 mm in the control group of this last study.
Horizontal:
After 3 months, Um et al.19 recorded decreases of -0.67 mm in the particulate dentin group, while, Joshi et al.21 recorded -0.15 mm at 4 months. These are an improvement when compared with those published in the classic Schropp et al. study2 , where dimensional changes were analysed after extraction without a graft, where losses were -3.8 mm at 3 months.
Pohl et al.18 and Del Canto-Díaz et al.17 measured these horizontal changes in procedures with particulate dentin at 4 months, 1 mm apical to the base of the bone crest and 3 mm apical to the base of the bone crest. Respectively, they reported losses of -1.38 mm and -0.46 mm at 1 mm from the crest, -0.82 mm and -0.31 mm at 3 mm from the crest, and -0.43 mm and -0.01 mm at 5 mm from the crest. Following this form of measurement in different planes of the crest, Cardaropoli et al.25 studied losses at the crest level (-1.3 mm) and at 3 mm from the crest (-0.9 mm) at 6 months after procedures with particulate dentin.
All these results are better than other studies detailed below, where xenograft or control groups were used and the measurements were also recorded at different points of the crest vertically. Matchei et al.22 reported decreases of -1.56 mm at 3 mm from the crest in the xenograft group at 4 months. In the control group of this same study, the losses were -2.96 mm at 6 mm from the crest, with larger losses (-0.56 mm in the xenograft group, and -1.81 mm in the control group), when compared with the particulate dentin groups. After 1 year, Valdec et al.23 reported losses of 1.1 mm in grafted alveoli with particulate dentin, rehabilitated with implants, which was much less than another study2 without grafts, which were as high as 50%.
Complications
Only one study14 reported complications after the alveolar preservation procedure with particulate dentin. These results are similar in studies which used a xenograft as biomaterial26, 27. This suggests high predictability and safety in treatment with particulate dentin.
New bone formation
The Andrade et al. study13 reported new bone formation of 26.3% at 4 months for the particulate dentin group, while Minetti et al.15 reported a range between 36.68% and 39.16%. These results exceed those obtained with allograft at 4 months, where the formation observed by Spinato’s 2014 study28 was between 18.84% and 23.3%. The results of the xenograft groups were also in this range at 4 months for the Matchei et al. study22 which reported 22.50%.
At 5 months, Andrade et al.13 reported up to 56.5% of new bone in particulate dentin groups, while Um et al.19 found 29.75% between 3 and 6 months. Particulate dentin gave higher percentages when compared with xenograft treated groups29.
At 6 months, the dentin results13,16 (31.24% and 66.5%, respectively) were similar to other studies where the groups were treated with autogenous bone (45.47%)20 or xenograft (25.7%)24.
Re-entry time
Re-entry was performed between 3 and 6 months in all studies. This waiting time is similar to studies with autologous graft20, xenograft22-29 and allgraft28; and lower than in other xenograft studies24. This leads us to think that the use of autogenous tooth has some properties at least as good as other widely used biomaterials. These results agree with the findings of the systematic review by De Risi et al.30 which concluded that alveoli grafted in alveolar preservation processes do not require a longer re-entry period than those healing spontaneously.
Current scientific evidence on the use of particulate dentin in alveolar preservation procedures is limited.
Of the few published studies identified, their sample size was low and the follow-up was short-term. Therefore, more and better studies are necessary.
Given the limitations of this bibliographic search, we can conclude that the use of particulate dentin is an alternative to other widely used biomaterials, with clear advantages over the lack of preservation procedures.
Jung RE, Philipp A, Annen BM y cols. Radiographic evaluation of different techniques for ridge preservation after tooth extraction: a randomized controlled clinical trial. J Clin Periodontol 2013; 40: 90-8.
Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restirative Dent 2003; 23: 313-23.
Araujo M, Linder E, Wennstrom J, Lindhe J. The influence of Bio-Oss Collagen on healing of an extraction socket: an experimental study in the dog. Int J Periodontics Restirative Dent 2008; 28: 123-35.
Barone A, Toti P, Quaranta A y cols. Clinical and Histological changes after ridge preservation with two xenografts: preliminary results from a multicentre randomized controlled clinical trial. J Clin Periodontol 2017; 44: 204-14.
Kim S, Kim H, Lim S. Combined implantation of particulate dentine, plaster of Paris, and a bone xenograft (Bio-Oss) for bone regeneration in rats. J Craniomaxillofac Surg 2001; 29: 282-8.
Calvo-Guirado JL, Ballester Montilla A, De Aza PN y cols. Particulated, Extracted Human Teeth Characterization by SEM– EDX Evaluation as a Biomaterial for Socket Preservation: An In Vitro Study. Materials 2019; 12, 380.
Bormann K, Suarez-Cunqueiro M, Sinikovic B y cols. Dentin as a suitable bone substitute comparable to ss-tcp–an experimental study in mice. Microvasc Res 2012; 84: 116-22.
Park SS, Kim SG, Lim SC, Ong JL. Osteogenic activity of the mixture of chitosan and particulate dentin. J Biomed Mater Res A. 2008; 87: 618-23.
Kim S, Yeo H, Kim Y. Grafting of large defects of the jaws with a particulate dentin–plaster of paris combination. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 88: 22-5.
Kim Y, Kim S, Byeon J, Lee H, Um I, Lim S, Kim S. Development of a novel bone grafting material using autogenous teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: 496-503.
Gomes MF, Abreu PP, Morosolli ARC, Araújo MM, Goulart MGV. Densitometric analysis of the autogenous demineralized dentin matrix on the dental socket wound healing process in humans. Braz Oral Res 2006; 20: 324-30.
Minamizato T, Koga T, Takashi I y cols.Clinical application of autogenous partially demineralized dentin matrix prepared immediately after extraction for alveolar bone regeneration in implant dentistry: a pilot study. Int J Oral Maxillofac Surg 2018; 47: 125-32.
Andrade C, Camino J, Nally M, Quirynen M, Martínez B, Pinto N. Combining autologous particulate dentin, L-PRF, and fibrinogen to create a matrix for predictable ridge preservation: A pilot clinical study. Clin Oral Investig 2019; 24: 1151-60.
Kim YK, Yun PY, Um IW. Alveolar ridge preservation of an extraction socket using autogenous tooth bone graft material for implant site development: prospective case series. J Adv Prosthodont 2014; 6: 521-7.
Minetti E, Giacometti E, Gambardella U y cols. Alveolar Socket Preservation with Different Autologous Graft Materials: Preliminary Results of a Multicenter Pilot Study in Human. Materials (Basel) 2020; 13(5): 1153.
Pang KM, Um IW, Kim YK, Woo JM, Kim SM, Lee JH. Autogenous demineralized dentin matrix from extracted tooth for the augmentation of alveolar bone defect: a prospective randomized clinical trial in comparison with anorganic bovine bone. Clin Oral Impl Res 2017; 27: 809-15.
Del Canto-Díaz A, De Elío-Oliveros J, Del Canto-Díaz M, Alobera-Gracia MA, Del Canto-Pingarrón M, Martínez-González JM. Use of autologous tooth-derived graft material in the post-extraction dental socket. Pilot study. Med Oral Patol Oral Cir Bucal 2019; 24: 53-60.
Pohl S, Binderman I, Tomac J. Maintenance of Alveolar Ridge Dimensions Utilizing an Extracted Tooth Dentin Particulate Autograft and PlateletRich Fibrin: A Retrospective Radiographic ConeBeam Computed Tomography Study. Materials (Basel) 2020; 13: 1083.
Um IW, Kim YK, Park JC, Lee JH. Clinical application of autogenous demineralized dentin matrix loaded with recombinant human bone morphogenetic-2 for socket preservation: a case series. Clin Implant Dent Relat Res 2019; 21: 4-10
Pelegrine AA, Da Costa CE, Correa ME, Marques Jr JF. Clinical and histomorphometric evaluation of extraction sockets treated with an autologous bone marrow graft. Clin Oral Implants Res 2010; 21: 535-42.
Joshi CP, Dani NH, Khedkar SU. Alveolar ridge preservation using autogenous tooth graft versus beta-tricalcium phosphate alloplast: A randomized, controlled, prospective, clinical pilot study. J Indian Soc Periodontol 2016; 20: 429-34.
Machtei EE, Mayer Y, Horwitz J, ZigdonGiladi H. Prospective randomized controlled clinical trial to compare hard tissue changes following socket preservation using allo- plasts, xenografts vs no grafting: clinical and histological findings. Clin Implant Dent Relat Res 2019; 21: 14-20.
Valdec S, Pasic P, Soltermann A, Thoma D, Stadlinger B, Rücker M. Alveolar ridge preservation with autologous particulated dentin-a case series. Int J Implant Dent 2017; 3:12.
Barone, A, Aldini, NN, Fini, M, Giardino, R, Calvo Guirado, JL, Covani, U. Xenograft versus extraction alone for ridge preservation after tooth removal: a clinical and histomorphometric study. J Periodontol 2008; 79: 1370-7.
Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L, Cardaropoli G. Socket preservation using bovine bone mineral and collagen membrane: a randomized controlled clinical trial with histologic analysis. Int J Periodontics Restirative Dent 2012; 32: 421-30.
Zhao L, Xu T, Hu W, Chung KH. Preservation and augmentation of molar extraction sites affected by severe bone defect due to advanced periodontitis: A prospective clinical trial. Clin Implant Dent Relat Res 2018; 20: 333-44.
Cha JK, Song YW, Park SH, Jung RE, Jung UW, Thoma DS. Alveolar ridge preservation in the posterior maxilla reduces vertical dimensional change: A randomized controlled clinical trial. Clin Oral Impl Res 2019; 30: 515-23.
Spinato S, Galindo-Moreno P, Zaffe D, Bernardello F, Soardi CM. Is socket healing conditioned by buccal plate thickness? A clinical and histologic study 4 months after mineralized human bone allografting. Clin Oral Implants Res 2014; 25: 120-6.
Milani S, Dal Pozzo L, Rasperini G, Sforza C, Dellavia C. Deproteinized bovine bone remodeling pattern in alveolar socket: a clinical immunohistological evaluation. Clin Oral Implants Res 2016; 27:295-302.
De Risi V, Clementini M, Vittorini G, Mannocci A, De Sanctis M. Alveolar ridge preservation techniques: a systematic review and meta-analysis of histological and histomorphometrical data. Clin Oral Impl Res 2015; 26: 50-68.

Fernández-Baca Cordón, Ignacio
DDS, MSc. Master’s in Oral Surgery, Implantology and Periodontics; Alfonso X El Sabio University.
De las Rivas Folqué, Teresa
DDS. Master’s student in oral surgery, implantology and periodontics; Alfonso X El Sabio University.
López-Malla Matute, Joaquín
DDS, MSc, PhD. Master’s Lecturer in Oral Surgery, Implantology and Periodontics; Department of Periodontics, Alfonso X El Sabio University.