Bibliographic review
Published in spanish Científica Dental Vol. 18. Nº 4. 2021 www.cientificadental.es
Physical properties of clinical utility of the new endodontics sealant cements based on silicates. Bibliographic review
Introduction: The obturation of the duct system plays a key role in the success of endodontic treatment. In an attempt to improve the properties of sealants cements, silicate-based sealants have recently been introduced to the market. Therefore, when carrying out the sealing of the duct system, it is useful to know the physical properties that the cement sealants present.
Objective: The objective of this work was to review the literature of the useful clinical physical properties that the new silicatebased cements present, and to compare them with the physical properties of the conventional epoxy resin-based cements.
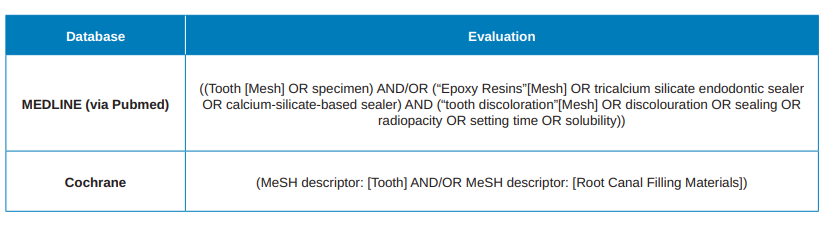
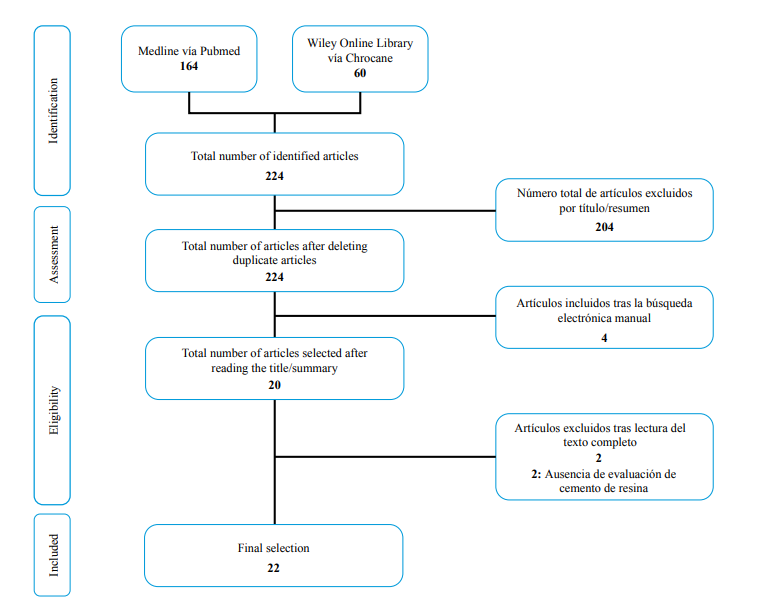
Material and method: After establishing the adapted research question, a literature review was carried out in two databases (Medline via Pubmed and Wiley Library via Chrocane Library) combining MeSH terms (Medical Subject Headings) and free terms.
In addition, a manual electronic search was carried out. The useful clinical physical properties selected were discoloration, sealing capacity, radiodensity, setting time and solubility.
Results: 224 potential studies were obtained. Finally, applying the inclusion and exclusion criteria, 22 studies were included in the review. The different studies compared the different physical properties of silicate-based cements, comparing them with resin-based cements.
Conclusions: Between silicate-based cements and resin cements, no differences in tooth discoloration were observed.
Nor differences were observed in sealing in most of the studies consulted. All the cements analysed presented radiodensity values within the recommended standards. Both the setting time and the solution depended on the type of cement evaluated. Some of the silicate-based cements showed higher solubility compared to resin-based cements.
To achieve success in endodontic treatment, it is necessary to obtain a complete obturation, after cleaning and conformation of the duct1 system. The materials commonly used in obturation are guttapercha and 2 sealants. Sealing cements are substances capable of penetrating between the obturation material and root canals3. There are different types available on the market, however, despite gathering many of the features described by Grossman, they do not manage to gather all4. They can be classified according to their main components5 in: zinc oxide–eugenol cement, calcium hydroxide cements, glass ionomer cements, silicone cements, resin cements or ceramic6 cements.
At present, cements composed of resins are the most used, being considered the epoxy resin cement AH PlusTM, the gold standard3,7. However, this cement presents a number of limitations such as a possible cytotoxicity, mutagenicity and inflammatory response8.
In addition, another limitation of this cement is the absence of bioactive properties9. Therefore, new types of sealants called bioceramic10 have recently been introduced to the market. These cements are based on the biological characteristics of MTA11 and include in their composition calcium silicates, calcium phosphates, calcium hydroxide and zirconium oxide as radiopacifier12. Therefore, the development of bioceramic cements has been based on obtaining a good biocompatibility. However, these cements must also have adequate physical properties4.
One of the physical properties that has gained importance in recent years is aesthetics7. The aesthetic result of the treatment of the opening is important, especially in the previous region13, since, although the access cavity is adequately prepared and cleaned with alcohol, there is a possibility that some cement sealant14 remains. On the other hand, the evaluation of the sealing capacity of new cement sealants is another property that has been considered an important parameter to consider5. The dimensional changes of the canal system, as well as the lack of adhesion of the gutta-percha, condition the achievement of complete sealing. Therefore, the adaptation of the sealing cement is a factor that influences the microfiltration and reinfection of the canal15 system. Another property considered essential is radiodensity, since it allows clinicians to distinguish between the materials used and adjacent anatomical structures16, as well as to assess the quality of the canal filler17. Another physical property that the clinician must take into account is the setting time. A slow or incomplete setting time may result in increased tissue irritation18, while a very short setting time may decrease the working time complicating and interfering with the obturation process19. Therefore, the setting time should be long enough to allow easy handling, especially in those sealing techniques that require more time20. Another property that has special relevance when evaluating sealants cements is the solubility21. Dissolution of the sealing cement could interfere with the quality of the canal treatment and trigger an inflammatory response of periapical tissues21,22. In addition, a vacuum could occur between the sealing material and the canal, increasing filtration over time21. Therefore, sealants should have a low solubility rate22.
Since there are different resin-based cements available on the market, it is important to know their physical properties. The objective of this literature review study was to analyse the scientific evidence of different physical properties of clinical applicability of different silicate-based sealants cements such as tooth discoloration, sealing capacity, radiodensity, setting time and solubility, and compare them with conventional resin-based cements.
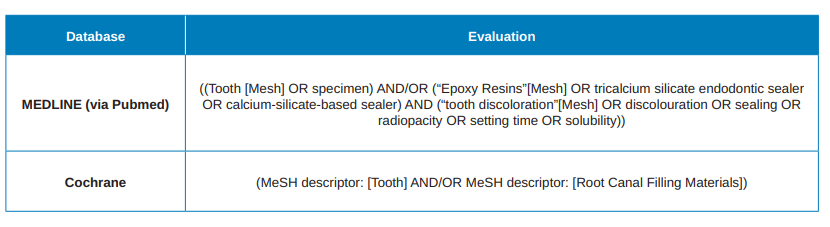
To carry out the present bibliographic review, taking into account the non-clinical nature of the studies, the following research PICO question was applied: In teeth or samples, silicate-based cements have better properties of discoloration, sealing, radiodensity and solubility compared to conventional cements based on epoxy resin? (Figure). The bibliographic search was carried out in the databases of Medline via PubMed and the Wiley Online Library via Cochrane Library. The search was performed by combining MeSH (Medical Subject Headings) terms with free terms, in a simple or multiple way and using Boolean operators. In vitro studies published between 2015 and 2021 were included. The last search was conducted on January 31, 2021. Studies evaluating cements that were not marketed or modified in the composition of marketed cements were excluded. Also excluded were those studies that compared obturation modifications of physical or technical properties. The search equations used in English are described in Table 1. In addition, a manual electronic search was conducted in the Journal of Endodontics, International Journal of Endodontics, Australian Endodontic Journal and Iranian Endodontic Journal.
A preliminary selection of the articles was made by the title and the summary. Duplicate articles were discarded. Then, the full text of the articles was obtained, excluding the articles that did not meet the established criteria. Manually selected articles were added and those that did not meet the criteria were excluded. The selected articles were grouped according to the analysed property. Those articles that analysed more than one property were identified and included in the corresponding groups. Taking into account the nature of the review, the characteristics of the studies were summarized in a descriptive way.
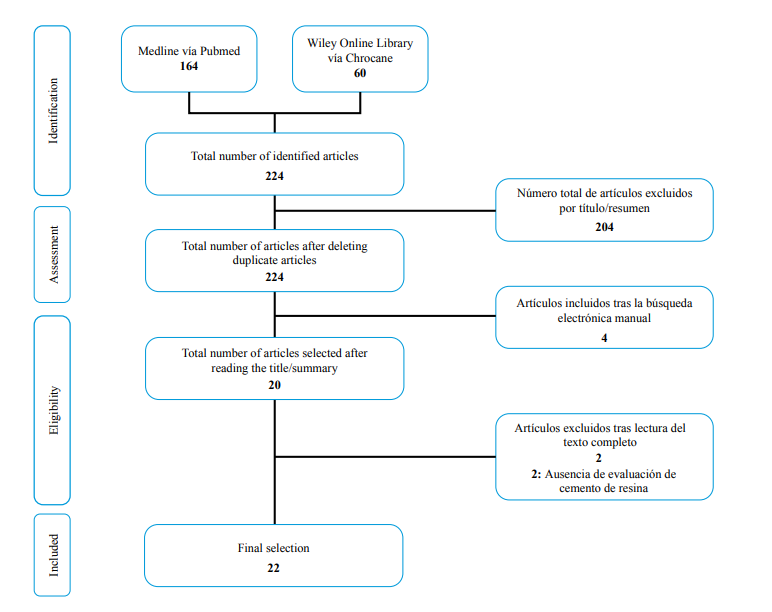
The flow chart that was used for the selection of the articles can be seen in the Figure. A total of 224 studies were identified in the initial search. No duplicate articles were found. After evaluating the titles and summaries of the studies obtained in the initial search, 204 studies were excluded because they did not meet the inclusion and exclusion criteria. Therefore, 20 studies were selected to read the full text, to which four more studies were added that were obtained by an electronic manual search. After reviewing the full text of the 24 studies, two were excluded because they did not include a comparative group of epoxy resin23,24.
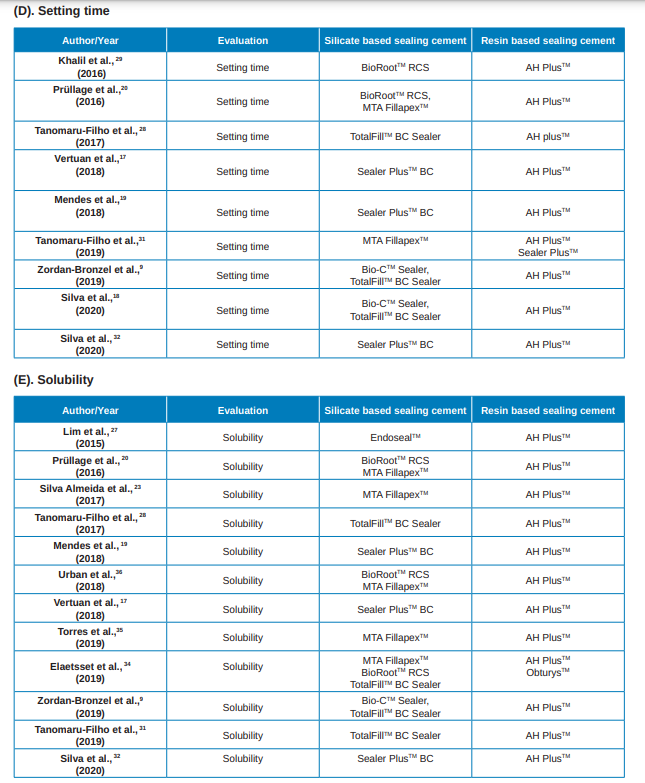
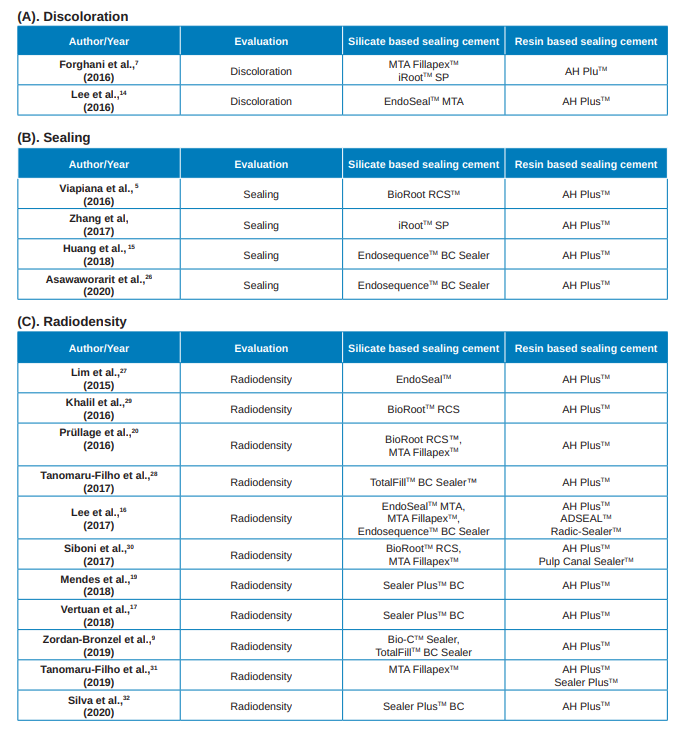
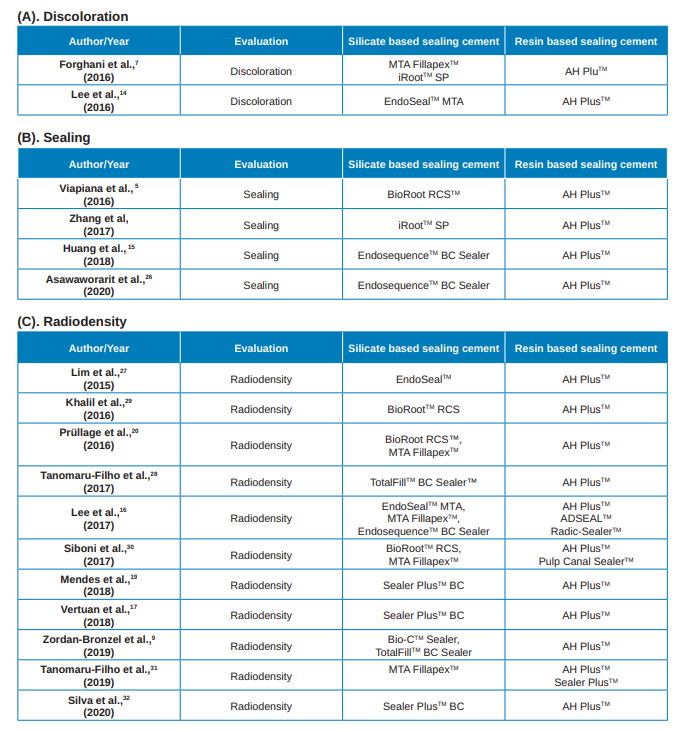
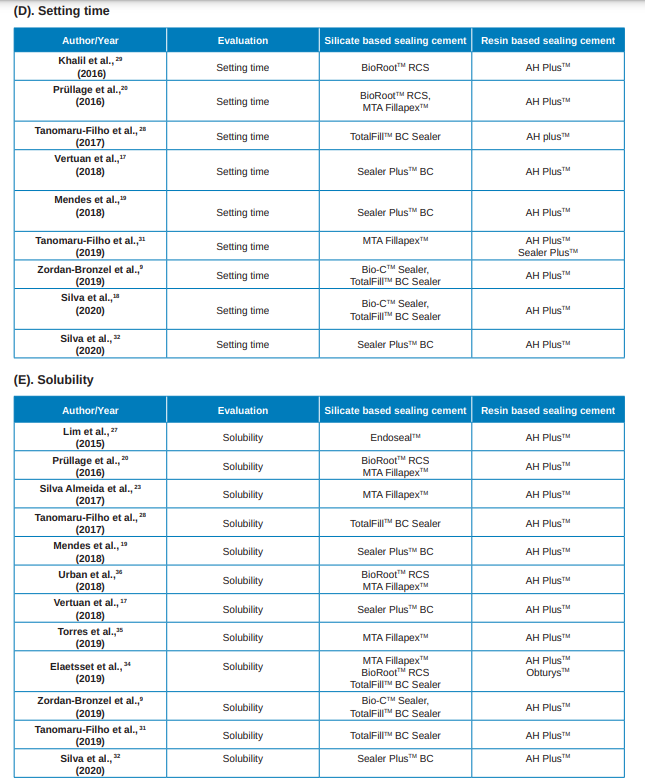
Therefore, the final number of articles included in the bibliographic review to carry out the data extraction was of 22. The studies were grouped according to the analysed property (Table 2): 2 discoloration (A); 4 sealing capacity (B); 11 radiodensity (C); 9 setting time (D); and 12 solubility (E). 9 articles analysed several properties.
The selected articles evaluated different physical properties of the new silicate-based sealing cements.
In order to evaluate the properties of the different cements, it is essential to establish standardized methodologies, so that the results can be reproduced and perform a reliable comparison of the data19.
Discoloration of dental tissue Studies that analysed the discoloration evaluated the same resin-based cement, the AH PlusTM7,14 sealant cement. However, different silicate-based cements were evaluated, being EndosealTM14, MTA FillapexTM and iRootTM SP7 the evaluated cements. Between both studies the discoloration of a total of 100 teeth was evaluated, including both bovine teeth14 and human teeth7. The technique used in the discoloration evaluation was spectrophotometry for both studies, using the CIELAB system. However, different evaluation periods were applied, 0-2 months14 and 0-6 months7.
The results obtained in the two selected studies did not find significant differences regarding discoloration between the analysed cements and the resin-based AH PlusTM. However, Forghani et al.,7 observed a progressive discoloration of all cements during the first three months after the cement application, with a tendency to decrease during the second quarter and up to the sixth month of the evaluation.
Sealing capability
The studies that evaluated the sealing of the new silicatebased sealants were45,15,25,26. Regarding the selected silicate cements, one study evaluated BioRootTM RCS5, two studies analysed EndoSequenceTM BC Sealer15,25 cement and one study iRootTM SP26 cement. All studies were based on the AH PlusTM resin cement.
In three of the selected studies5,15,26 there were no differences in sealing capacity between silicate-based cement and epoxy resin-based cement. On the other hand, in one of the studies26, a better seal was obtained with EndosequenceTM BC Sealer silicate cement than with epoxy resin cement. Radiodensity
Eleven studies9,16,17,19,20,27-32 were selected that evaluated the radiodensity of silicate-based cements, comparing them with epoxy resin-based cements. The silicate-based cements analysed in the studies were: EndoSequenceTM BC Sealer16, EndoSealTM MTA16,28, TotalFillTM BC Sealer9,30, BioRootTM RCS20,29,31, MTA FillapexTM16,20,31,32, Sealer PlusTM BC17,19,27 and BioCTM Sealer9. All studies evaluated cement based on epoxy resin AH PlusTM. In addition, two studies also included epoxy resin-based cements ADSEALTM, Radic-SealerTM16 and Sealer PlusTM32.
The American National Standards Institute and the American Dental Association (ADA) in their specification number 57 of the year 2000 establish a minimum radiodensity equivalent to 3.00 mm AI33. The standard established by the International Organization for Standardization (ISO) 6878 also specifies that the radiodensity must be equal to or greater than 3 mm AI31. All the cements evaluated presented radiodensity values within the recommended ISO standards.
In most studies AH PlusTM cement presented higher radiodensity values than BioRootTM RCS29,31, TotalFillTM BC9,30, Bio-CTM Sealer9, EndosequenceTM BC Sealer16, Sealer PlusTM BC17,19,27, MTA FillapexTM9,30,32 and EndosealTM28. How ever, in other studies, there were no significant differences between AH PlusTM and
BioRootTM RC, MTA FillapexTM20 and EndoSealTM MTA16 cements. In studies that also analysed other resinbased cements, radiodensity results with respect to silica-based cements were similar. The MTA FillapexTM cement showed lower radiodensity than the resin cements Sealer PlusTM9, Pulp Canal SealerTM31, RadicSealerTM and AD SealTM16.
Similarly, BioRootTM RCS cement showed a lower radiodensity compared to the Pulp Canal SealerTM31 resin cement. On the other hand, the EndosequenceTM BC Sealer cement also presented a lower radiodensity compared to Radic SealerTM cement. However, the EndosequenceTM BC Sealer cement presented a higher radiodensity than the AD SEALTM16 resin cement.
When evaluating the radiodensity differences between silicate-based cements, the results differ between the studies and depending on the analysed cements.
One study observed greater radiodensity with MTA FillapexTM compared to BioRootTM RCS31. However, in another study, no differences were obtained between the two cements20, nor between the cements BioCTM Sealer and TotalFillTM BC Sealer9. The only study that analysed three silicate-based cements16 showed different radiodensity values between cements, with EndoSealTM MTA cement being the largest, followed by EndosequenceTM BC Sealer and MTA FillapexTM. The differences in radiodensity could be caused by the presence of different radiopacifying agents in the composition of the cements16.
Setting time
The 9 selected studies9,17-20,27,29,30,32 evaluated the setting time through needles that were introduced in the cement models, as established in IS0 687619 ANSI/ ADA 5727 standard.
The following silicate-based cements were evaluated: BioRootTM RCS20,29; Sealer PlusTM17,18,27; TotalFillTM BC Sealer, Bio-CTM Sealer9,18,30; and MTA FillapexTM20,32. In all studies, the setting time results of silicate-based cements were compared with AH PlusTM epoxy resin cement. One study also analysed Sealer PlusTM32 cement.
Two studies analysed the setting time of the BioRootTM RCS20,29 cement. Both observed that BioRootTM RCS had a setting time lower than that of the resin-based cement AH PlusTM20,29. In one of the two studies20, they also evaluated the setting time of the MTA FillapexTM cement, which was completed in one week, the evaluation period established in the study. In another study, MTA FillapexTM had a higher setting time than AH PlusTM and PlusTM32 Sealer cements.
Three studies evaluated Sealer PlusTM BC17,19,27 silicate cement. Similar to the results observed with BioRootTM RCS cement, Sealer PlusTM BC also presented a lower setting time than AH PlusTM17,19,27 epoxy resin cement. In two studies18,30 TotalFillTM BC Sealer cement was analysed. In both, the setting time of silicate-based cement was lower than that of AH PlusTM. However, the two studies that analyse Bio-CTM Sealer cement presented differences in the results from each other.
In one study AH PlusTM cement had a shorter working time compared to Bio-CTM Sealer9, while in the other study18, epoxy resin-based cement AH PlusTM had a longer setting time lower than Bio-CTM Sealer.
When analysing the setting time of silicate cements, in one study20 there were no differences observed between BioRootTM RCS and MTA FillapexTM cements, while two studies observed a shorter setting time of Bio-CTM Sealer cement compared to TotalFillTM BC Sealer9,18. This cement in one of the 18 studies did not set after the 25 days established in the study conditions.
Solubility
Twelve articles evaluated the solubility of the sealants cements by comparing it with the solubility of the epoxy resin cements5,9,17,19,20,27,28,30,34-37.
The selected studies analysed silicate-based cements: BioRootTM RCS20,34,37; MTA FillapexTM20,32,34-37; TotalFillTM BC Sealer9,30,34; Sealer PlusTM BC17,19,27,33; Bio-CTM Sealer9; and EndosealTM28. All articles used as control group the AH PlusTM resin cement. Two articles, in addition to the AH PlusTM cement, analysed the properties of the ObturysTM34 and Sealer PlusTM32 cements.
Differences were observed, both between the different silicate-based cements as between the evaluation periods, in relation to resin-based cements. The BioRootTM RCS cement presented higher solubility than the AH PlusTM20,34,37 and ObturysTM34 resin cements. The Bio-CTM Sealer cement also showed higher solubility than the AH PlusTM9 cement.
Similarly, TotalFillTM BC Sealer cement obtained greater solubility than AH PlusTM resin cement in most of the analytical periods in the different studies9,30,34.
However, in the first evaluation period of a study34, no significant differences were observed between BioRootTM RCS and AH PlusTM and ObturysTM resinbased cements. On the other hand, in most studies and periods analysed of the MTA FillapexTM cement, a higher solubility was observed compared to resin cements20,32,34,35,37. However, one study observed greater solubility of MTA FillapexTM compared to AH PlusTM at two hours of evaluation20. On the other hand, different studies did not show any differences regarding solubility between the two cements during the first minute of evaluation20, at 24 hours34 and after a week34,36. However, studies that analysed longer evaluation periods, the solubility of MTA FillapexTM cement was superior to that of resin cement32,35,37.
On the other hand, the silicate cement Sealer PlusTM BC obtained contradictory results. In one study19 presented greater solubility than AH PlusTM, while in two studies there were no differences between both17,27.
Similarly, the only study that analysed the EndosealTM28 cement did not obtain solubility differences with respect to AH PlusTM resin cement in the analysed period.
When evaluating the solubility between the different silicate-based cements different results were observed between the different evaluation periods. Bio-CTM Sealer cement presented higher solubility than the TotalFillTM BC Sealer9 cement. On the other hand, in one study there were no significant differences in the different periods between TotalFillTM BC Sealer, MTA FillapexTM and BioRootTM RCS cements, except in the first evaluation period (24 hours), in which, the BioRootTM RCS cement presented higher solubility than the MTA FillapexTM34. However, the solubility of both cements differs between studies, since greater solubility can be observed of MTA FillapexTM compared to BioRootTM RCS20, as greater solubility of BioRootTM RCS cement compared to MTA FillapexTM37. Further research would be needed to analyse the solubility of both cements in the long term.
Taking into account the lack of long-term clinical studies and the limitations of in vitro studies, the physical properties of new silicate-based sealants can guide the dentist in the selection of the sealing cement.
There were no differences in tooth discoloration between silicate-based and epoxy resin-based cements. Neither were differences observed between both types of cements, regarding sealing, in most of the studies selected in the present work.
Both epoxy resin-based cement and silicate-based cements presented radiodensity values within the recommended ISO standards. The setting time of silicate-based cements, compared with resin cements, varied depending on the type of cement. Although solubility varied according to the cement type and the evaluation period, some of the silicate-based cements showed higher solubility than resin-based cements.
Troiano G, Perrone D, Dioguardi M,
Buonavoglia A, Ardito F, Lo Muzio L. In vitro evaluation of the cytotoxic activity of three epoxy resin-based endodontic sealers. Dent Mater J 2018;37:374–8.
Dimitrova-Nakov S, Uzunoglu E,
Ardila-Osorio H, Baudry A, Richard G,
Kellermann O, y cols. In vitro bioactivity of BiorootTM RCS, via A4 mouse pulpal stem cells. Dent Mater 2015;31:1290–7.
Piai GG, Duarte MAH, Nascimento AL
do, Rosa RA da, Marcus Vinícius Reis
S, Vivan RR. Penetrability of a new
endodontic sealer: A confocal laser scanning microscopy evaluation. Microsc Res Tech 2018;81:1246–9.
Zhou HM, Du TF, Shen Y, Wang ZJ, Zheng YF, Haapasalo M. In vitro cytotoxicity of calcium sSilicate-containing endodontic sealers. J Endod [Internet]. 2015;41:56– 61.
Viapiana R, Moinzadeh AT, Camilleri
L, Wesselink PR, Tanomaru Filho M,
Camilleri J. Porosity and sealing ability of root fillings with gutta-percha and BioRoot RCS or AH Plus sealers. Evaluation by three ex vivo methods. Int Endod J 2016;49:774–82.
Jafari F, Jafari S. Composition and
physicochemical properties of calcium
silicate based sealers: A review article. J Clin Exp Dent. 2017;9:e1249–55.
Forghani M, Gharechahi M, Karimpour S.
In vitro evaluation of tooth discolouration induced by mineral trioxide aggregate Fillapex and iRoot SP endodontic sealers. Aust Endod J. 2016;42:99–103.
Lim M, Jung C, Shin D-H, Cho Y, Song M. Calcium silicate-based root canal sealers: a literature review. Restor Dent Endod. 2020;45:1–17.
Zordan-Bronzel CL, Esteves Torres FF, Tanomaru-Filho M, Chávez-Andrade GM, Bosso-Martelo R, Guerreiro-Tanomaru JM. Evaluation of physicochemical properties of a new calcium silicate–based sealer, Bio-C Sealer. J Endod. 2019;45:1248–52.
Munitić MS, Peričić TP, Utrobičić A,
Bago I, Puljak L. Antimicrobial efficacy of commercially available endodontic bioceramic root canal sealers: A systematic review. PLoS One. 2019;14:1–20.
Colombo M, Poggio C, Dagna A, Meravini MV, Riva P, Trovati F, et al. Biological and physico-chemical properties of new root canal sealers. J Clin Exp Dent. 2018;10:e120–6.
Bueno CRE, Valentim D, Marques
VAS, Gomes-Filho JE, Cintra LTA,
Jacinto RC, y cols.. Biocompatibility
and biomineralization assessment
of bioceramic-, epoxy-, and calcium
hydroxide-based sealers. Braz Oral Res. 2016;30:1–9.
Kohli MR, Yamaguchi M, Setzer FC,
Karabucak B. Spectrophotometric
analysis of coronal tooth discoloration
induced by various bioceramic cements and other endodontic materials. J Endod [Internet]. 2015;41:1862–6.
Lee DS, Lim MJ, Choi Y, Rosa V, Hong
CU, Min KS. Tooth discoloration induced by a novel mineral trioxide aggregatebased root canal sealer. Eur J Dent. 2016;10:403–7.
Huang Y, Orhan K, Celikten B, Orhan
AI, Tufenkci P, Sevimay S. Evaluation of the sealing ability of different root canal sealers: A combined SEM and micro-CT study. J Appl Oral Sci. 2018;26:1–8.
Lee JK, Kwak SW, Ha JH, Lee WC,
Kim HC. Physicochemical properties of epoxy resin-based and bioceramic-based root canal sealers. Bioinorg Chem Appl. 2017;2017:1–9.
Vertuan GC, Duarte MAH, Moraes IG de, Piazza B, Vasconcelos B de C, Alcalde MP, y cols. Evaluation of Physicochemical Properties of a New Root Canal Sealer. J Endod [Internet]. 2018;44:501–5.
Silva EJNL, Ehrhardt IC, Sampaio GC,
Cardoso ML, Oliveira D da S, Uzeda MJ, y cols. Determining the setting of root canal sealers using an in vivo animal experimental model. Clin Oral Investig. 2021;25:1899–906.
Mendes AT, Silva PB da, Só BB,
Hashizume LN, Vivan RR, Rosa RA da, et al. Evaluation of physicochemical properties of a new calcium silicate–based sealer, Bio-C Sealer. Braz Dent J. 2018;29:536–40.
Prüllage RK, Urban K, Schäfer E,
Dammaschke T. Material properties of a tricalcium silicate–containing, a mineral trioxide aggregate–containing, and an epoxy resin–based root canal sealer. J Endod. 2016;42:1784–8.
Silva EJ, Perez R, Valentim RM,
Belladonna FG, De-Deus GA, Lima
IC, y cols. Dissolution, dislocation and
dimensional changes of endodontic
sealers after a solubility challenge:
a micro-CT approach. Int Endod J.
2017;50:407–14.
Silva EJNL, Cardoso ML, Rodrigues JP, De-Deus G, Fidalgo TK da S. Solubility of bioceramic- and epoxy resin-based root canal sealers: A systematic review and meta-analysis. Aust Endod J. 2021:1–13.
Kharouf N, Arntz Y, Eid A, Zghal J, Sauro S, Haikel Y, y cols. Physicochemical and Antibacterial Properties of Novel, Premixed Calcium Silicate-Based Sealer Compared to Powder–Liquid Bioceramic Sealer. J Clin Med. 2020;9:3096.
Oh S, Cho SI, Perinpanayagam H, You J, Hong SH, Yoo YJ, y cols. Novel calcium zirconate silicate cement biomineralize and seal root canals. Materials (Basel). 2018;11:1–11
Asawaworarit W, Pinyosopon T,
Kijsamanmith K. Comparison of apical
sealing ability of bioceramic sealer and
epoxy resin-based sealer using the
fluid filtration technique and scanning
electron microscopy. J Dent Sci [Internet]. 2020;15:186–92.
Zhang N, Li X, Miao LY, Wu J, Liu C,
Yang WD. Study on the sealing ability of biological root canal sealer iRoot SP in root canal filling. Shanghai Kou Qiang Yi Xue. 2017; 1;26:395–8.
Silva EJ, Hecksher F, Vieira VT, Vivan RR, Duarte MA, Brasil SC, y cols. Cytotoxicity, antibacterial and physicochemical properties of a new epoxy resinbased endodontic sealer containing calcium hydroxide. J Clin Exp Dent. 2020;12:e533–9.
Lim ES, Park YB, Kwon YS, Shon WJ,
Lee KW, Min KS. Physical properties and biocompatibility of an injectable calciumsilicate-based root canal sealer: In vitro and in vivo study. BMC Oral Health [Internet]. 2015;15:1–7.
Khalil I, Naaman A, Camilleri J. Properties of Tricalcium Silicate Sealers. J Endod [Internet]. 2016;42:1529–35.
Tanomaru-Filho M, Torres FFE, ChávezAndrade GM, de Almeida M, Navarro LG, Steier L, y cols. Physicochemical properties and volumetric change of silicone/bioactive glass and calcium
silicate–based endodontic sealers. J
Endod. 2017;43:2097–101.
Siboni F, Taddei P, Zamparini F, Prati
C, Gandolfi MG. Properties of bioroot
RCS, a tricalcium silicate endodontic
sealer modified with povidone
and polycarboxylate. Int Endod J.
2017;50(Special Issue 2):e120–36.
Tanomaru-Filho M, Prado MC, Torres FFE, Viapiana R, Pivoto-João MMB, GuerreiroTanomaru JM. Physicochemical properties and bioactive potential of a new epoxy resin-based root canal sealer.
Braz Dent J. 2019;30:563–8.
Marín-Bauza GA, Silva-Sousa YTC, da
Cunha SA, Rached FJA, Bonetti-Filho I, Sousa-Neto MD, et al. Physicochemical properties of endodontic sealers of different bases. J Appl Oral Sci. 2012;20:455–61.
Elyassi Y, Moinzadeh AT, Kleverlaan CJ. Characterization of leachates from 6 root canal sealers. J Endod. 2019;45:623–7.
Torres FFE, Guerreiro-Tanomaru JM,
Bosso-Martelo R, Espir CG, Camilleri
J. Solubility , Porosity, dimensional and volumetric change of endodontic sealers. Braz Dent J. 2019;30:368–73.
6. Silva Almeida LH, Moraes RR, Morgental RD, Pappen FG. Are premixed calcium silicate–based endodontic sealers comparable to conventional materials?
A systematic review of in vitro studies. J Endod. 2017;43:527–35
Urban K, Neuhaus J, Donnermeyer D,
Schäfer E, Dammaschke T. Solubility and pH value of 3 different root canal sealers: A Long-term Investigation. J Endod. 2018;44:1736–40.

Parziale, Isabella
Graduated in Dentistry from the European University of Madrid
Freire Mancebo, Yolanda
Assistant Professor of the PreClinical Dentistry Department of the European University of Madrid.
Díaz-Flores García, Víctor
Assistant Professor of the PreClinical Dentistry Department of the European University of Madrid.