Original article
Published in spanish Científica Dental Vol. 19. Nº 3. 2022
www.cientificadental.es
Implants of 4.5 and 5.5 mm length inserted directly in crestal elevation with autologous bone attached to PRFG-Endoret in residual bone heights of 2-3 mm: retrospective study
Introduction. The approach to the atrophic maxilla in height is a challenge for the odontologist, new techniques are increasingly becoming more common that allow us to place implants with less invasiveness for the patient. The incorporation of the transcrestal approach and the decrease in the length of the implants have been key to bring the treatment to more patients with a smaller number of surgical interventions. In this study we show a number of cases with extreme height bone atrophy rehabilitated by transcrestal elevation and implants of 4.5 and 5.5 mm in length.
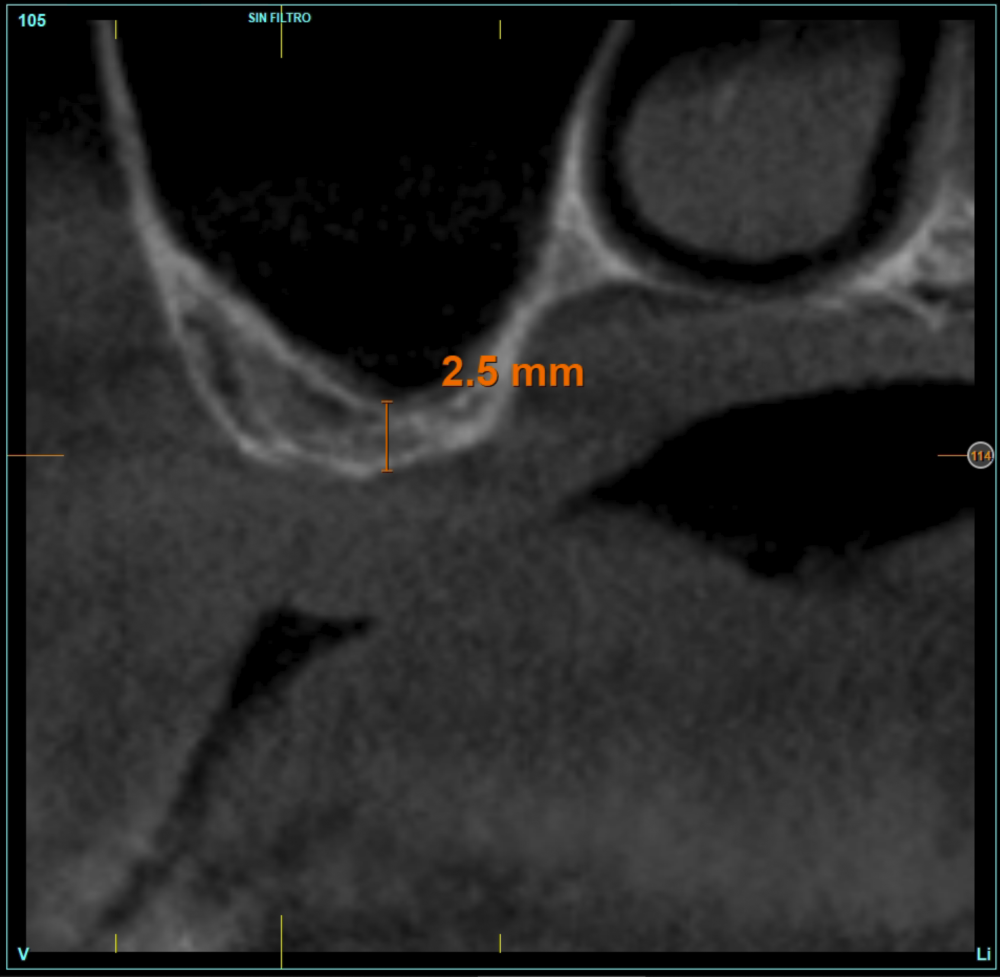
Material and method. A retrospective study has been carried out in patients in whom extra-short implants (4.5 and 5.5 mm length) were inserted directly by transcrestal elevation with residual ridges between 2 and 3 mm. The implant was the analysis unit for the descriptive statistics regarding location, implant dimensions, and radiographic measurements. The patient was the measurement unit for the analysis of age, sex and medical history. The main variable was the gain in height over the apex of the implant after 6 months of the surgery and one year after the load comparing both measurements and as secondary variables the biological complications and the implant failure were recorded.
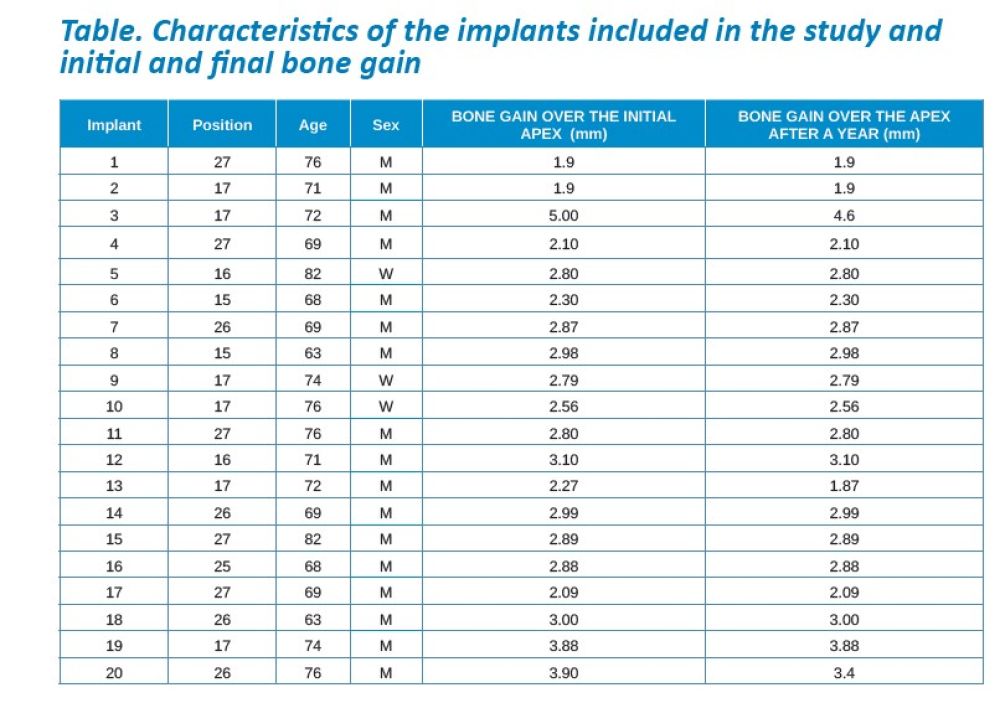
Results. Ten patients who met the inclusion criteria were recruited and 20 implants were inserted. The mean residual bone volume height was 3.1 mm (+/- 0.3 mm with a range elevation above the apex of the implant in millimetres is of 2.8 mm (+/- 0.99 range 1.9 -5 mm). In the control cone-beam after one year of the studied load of the implants, the bone gain achieved was maintained, with no decrease in the volume gained, only three cases showed a decrease of between 0.4 and 0.5 mm of the initial volume at the end. No implants failed in the follow-up period and no biological complications were found in the surgery.
Conclusions. Achieving success of implants placed in areas of extreme horizontal atrophy by transcrestal sinus approach with extra-short implants is possible, provided that a correct stabilization of the implant is achieved in the initial phase (primary stability) and a careful milling protocol is used, insertion of the implant, graft management, 100% processing of bone and autologous plasma and subsequent loading of the same (progressive load).
In implantology, as in other areas of medical medicine, surgical techniques undergo an evolution, usually to adapt to new scientific advances to new materials and to achieve techniques that solve the same problems in less time, more predictability and with lower morbidity for the patient1-3. The advent of shorter implants such as short, extra-short and ultra-short has made possible the rehabilitation of large height atrophies with fewer surgeries, avoiding, in many cases, accessory bone regeneration techniques4-9. In the posterior areas of the maxilla, the most used technique to produce a gain in hight when bone has been lost vertically has long been sinus elevation by lateral approach10. Subsequently, a variant of this technique was developed, generating access through the alveolar crest, from the neo alveolus formed for the insertion of the future implant. This technique initially described by Summers11, which received his name, used osteotomes and hammer to raise the lower cortical of the sinus floor once the approach was made through the crest. As a result of achieving a constant improvement of the crestal approach surgery, different access systems (ultrasound and milling cutters mainly)12,13 and alternatives designed to detach the Schneider membrane once exposed (controlled pressure instruments, pneumatic balloons, spatulas with different shapes…)14-15, as well as variations regarding the type of material used as a graft, even performed out without filling material18-20.
The crestal lifting technique is currently among the most used to treat the height deficit of the posterior maxilla, when there is a bone remnant of at least 5 mm21-23 in height, although currently there are also research studies that indicate that this technique can be used even if the bone volume is less than this height20-25.
The use of a careful milling technique adapted to the receiving orifice, increasing the primary stability with the diameter of the implant and the anchorage in the vestibular cortex, palatal, mesial and distal (instead of looking for apical anchorage), they are the success keys of these works where extra-short implants have been inserted at residual heights of less than 5 mm even when the residual density was low20-25. In addition, in the follow-up of these implants, no lower success rate or complications related to low residual height or migrations of implants to the maxillary sinus have been 20-25.
In this type of approach to the sinus, an important point is the stability of the grafted bone, located above the apex of the implant and with a bone tissue little vascularized (as usually occurs in these large atrophies with low density), so assessing what happens with the bone volume gained by this long-term procedure is also a key fact26,27. The mineralization of the bone graft and its maintenance once the implant loading is performed can make the difference in the success of the technique, especially in increasingly extreme cases. Therefore, the material used as a graft and the surface of the implant are two factors to take into account when performing this type of procedure28-31. Hydrophilic and osteoconductive surfaces in implants are of vital importance in these complex cases, as well as the filling materials that stimulate the formation of new bone28-31. The implants with UnicCa (Biotechnology Institute, Vitoria, Spain) surface, have a superhydrophilic surface. It is a very rough surface (Optima), with a calcium ions layer. This implies that the contact of blood and plasma with all points of the surface increases to the maximum the active surface for regeneration, by being completely coated with fluids due to its high capillarity. In the following series of clinical cases, patients treated by transcrestal sinus lift, with extra-short and ultra-short implants (4.5 and 5.5 mm), BTI (Biotechnology institute), of internal connection and universal plus platform in residual bone heights below 3 mm, studying the behaviour of implants regarding their survival as well as the maintenance of the bone volume achieved in the crestal elevation.
Patients were retrospectively selected in which extra-short implants were inserted using the crestal lift technique using frontal drills, according to the technique used and described by our study group13, which surgery was carried out before 2015 to have a load follow-up period of at least 5 years, and in which the residual bone height was less than 3 mm.
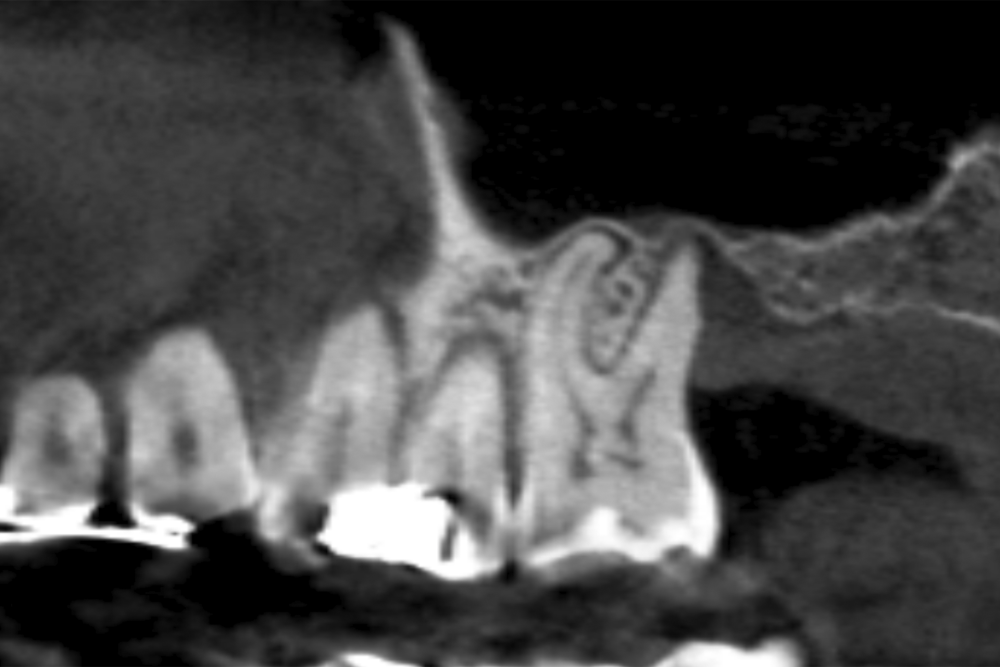
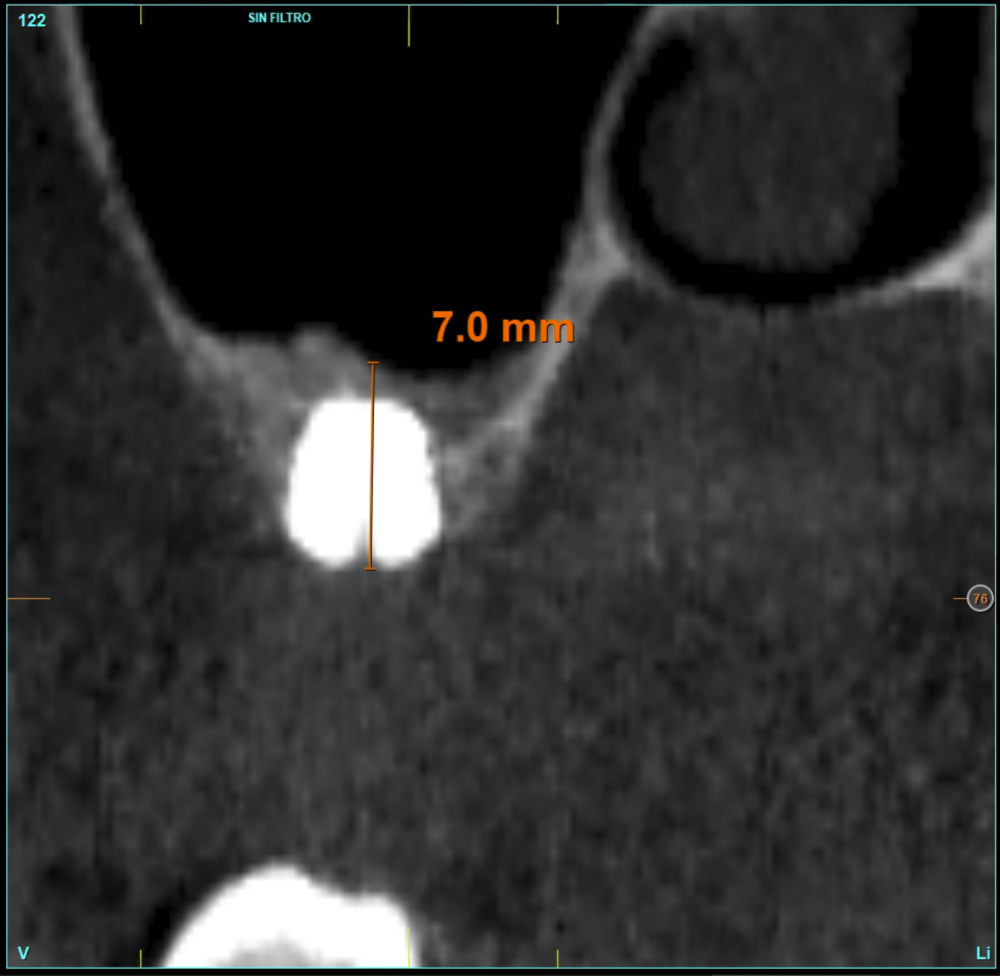
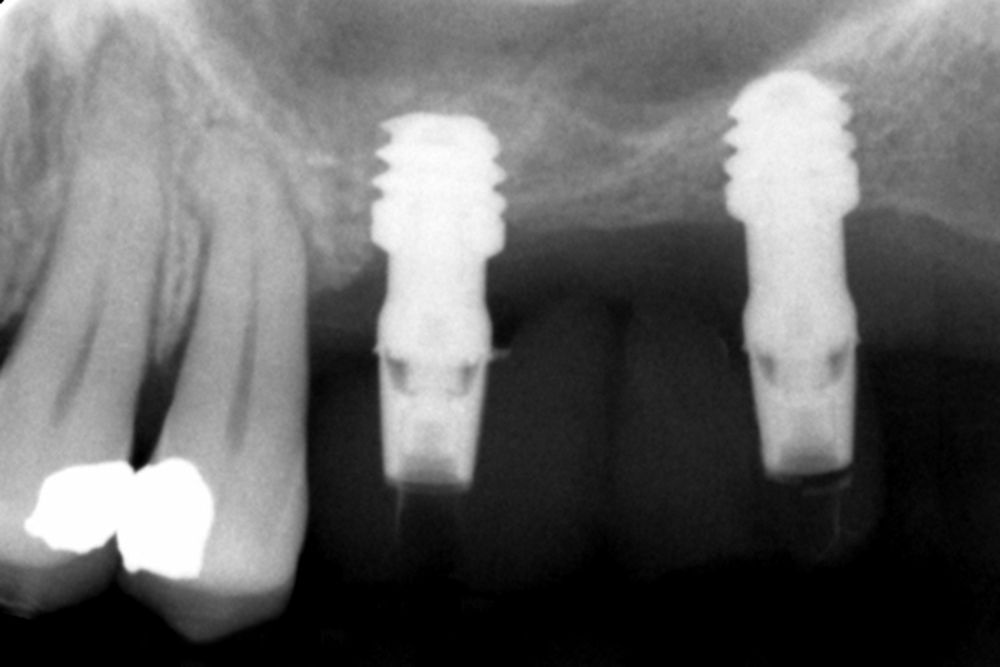
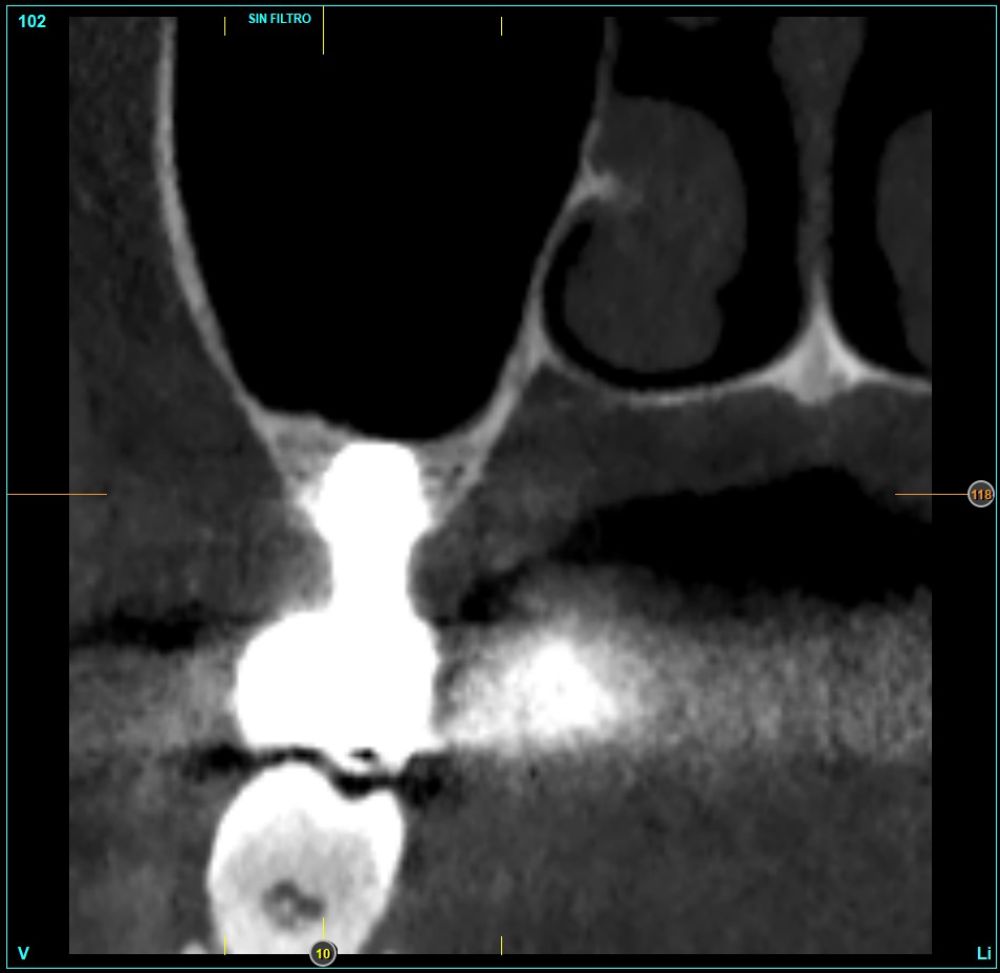
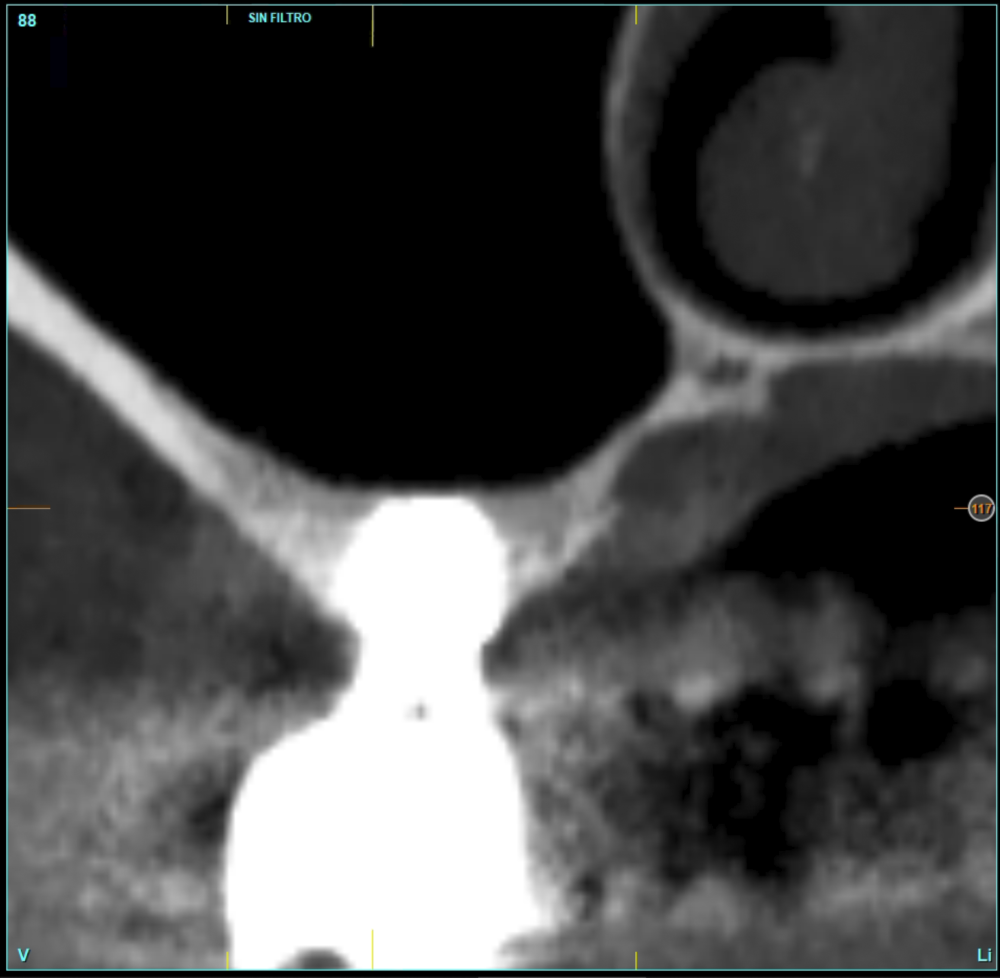
In all cases, a diagnosis was made based on study models, intraoral examination of the patient and performing a Cone-beam analysed using the specific BTI-Scan 3 software (Biotechnology Institute, Vitoria, Alava, Spain).
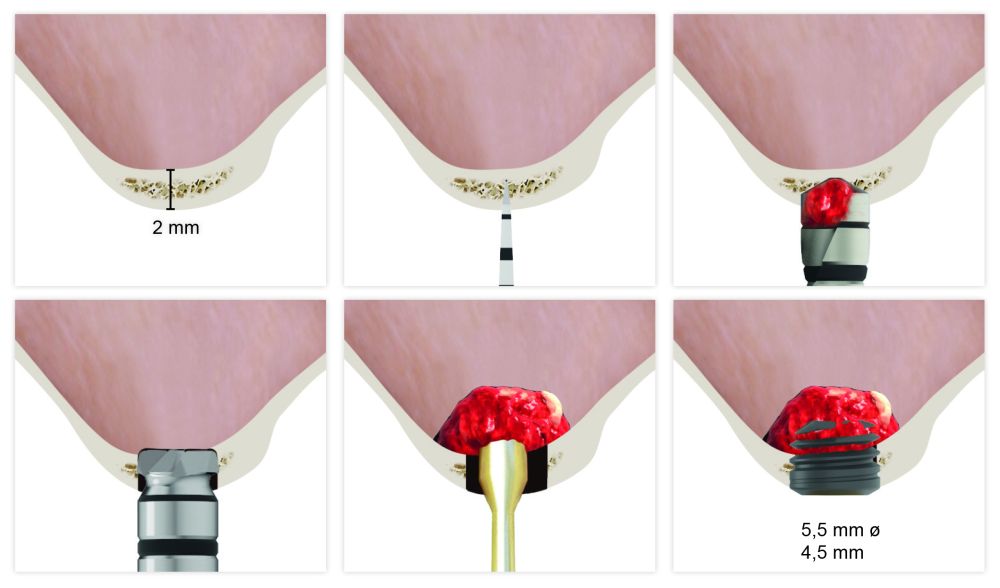
Prior to the implant insertion, an antibiotic premedication consisting of amoxicillin 2 g orally one hour before the procedure and paracetamol 1 g orally (as analgesic) was used. Patients continued with an amoxicillin treatment 500- 750 mg orally every 8 hours (depending on weight) for 5 days. As a filling material in all cases, using the autologous bone obtained from the milling (from the same transcrestal elevation area where the implants were inserted simultaneously) embedded in PRGF-Endoret fraction 2. The milling was carried out at low revolutions (biologic milling)32, the membrane is accessible by crestal perforation, it is detached, the graft is placed and then the implant is inserted with the surgical motor fixed at 25 Ncm and 25 rpm, finishing the implant insertion with the torque wrench (Figure 1).
Patients attend subsequent check-ups performing a control Cone-Beam after 5 months (before loading the implant) and after one year of the load, performing a new measurement in these images to analyse the bone gain and the maintenance of the same. In these check-ups, data are collected on prosthetic complications or crestal bone loss in these patients, as well as possible failures.
The implant was the analysis unit for the descriptive statistics regarding location, implant dimensions, and radiographic measurements. The patient was the measurement unit for the analysis of age, sex and medical history. The main variable was the gain in height over the apex of the implant after 6 months of surgery and one year after the load comparing the two measurements and the biological complications and implant failure were recorded as secondary variables. The Shapiro-Wilk test was performed on the data obtained to verify the normal distribution of the sample.
The qualitative variables were described using a frequency analysis. Quantitative variables were described by average and standard deviation. Implant survival was calculated using the Kaplan-Meier method. The data were analysed with SPSS v15.0 for Windows (SPSS Inc., Chicago, IL, USA).
Ten patients who met the inclusion criteria were recruited, in which 20 implants were inserted. Three of them were women with an average age of 72 (+/- 6 years). None of the patients were smokers at the time of surgery and did not have any active periodontal disease. The majority of the implants diameter included in the study was 5 mm (60%), followed by 4.5, 5.5 and 4.75 mm (13.33% each). The predominant length was 5.5 mm (86.6% of the cases), with 13.4% of the remaining implants with a length of 4.5 mm. The most common positions were for the second molars (molars 27 and 17) representing 55% of the cases.
The mean height of the residual bone volume was 3.1 mm (+/- 0.3 mm with a range of 3-4 mm). In all cases, transcrestal sinus elevation was performed, with particulate autologous bone obtained from milling the neo alveolus generation zone for implant insertion, being the average of this elevation above the apex of the implant of 2.8 mm (+/- 0.99 range 1.9 -5 mm). In the CT control scan after one year of inserting the studied implants, the bone gain achieved was maintained, no decrease in the volume gained was observed, only three cases showed a decrease of between 0.4 and 0.5 mm of the initial volume at the end (Table).
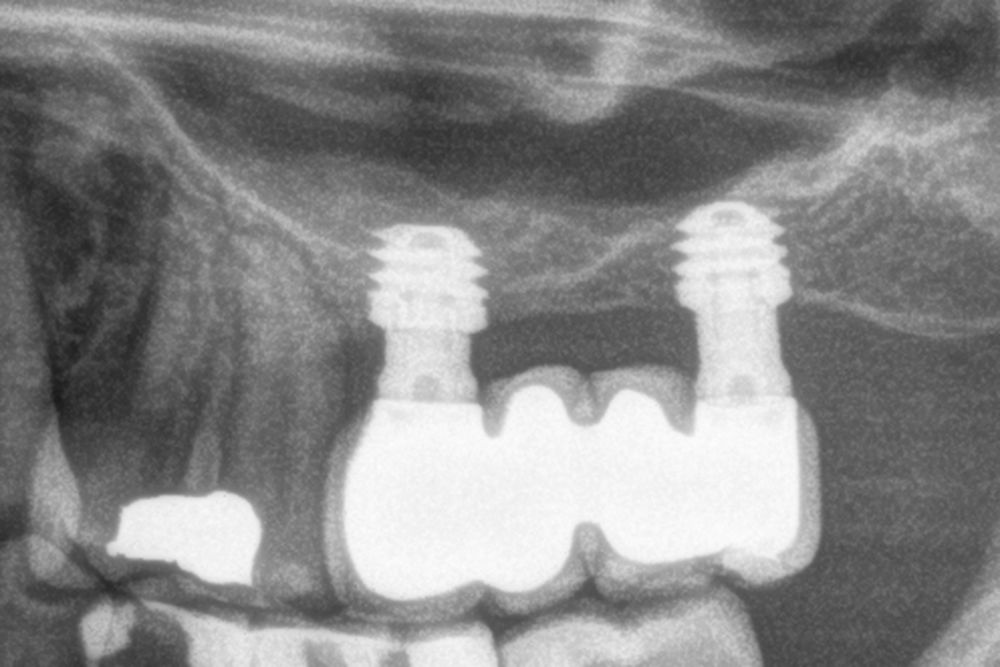
All implants were rehabilitated in two phases and all of them were ferulized to other implants in the rehabilitation. In all cases, screwed prostheses of more than one implant with intermediate elements (transepithelial) were performed, ferulizing to other implants with a length of 4.5 or 5.5 mm. In all situations, a progressive prosthesis load was carried out 6 months after insertion of the implant consisting of a provisional structure finished in resin to move to a definitive metal-ceramic prosthesis. In all cases, the initial transepithelial are preserved to maintain the hermeticity achieved in the first phase of prosthesis manufacture.
No implants failed in the follow-up period and no biological complications were found in the surgery. The postoperative condition of all patients was excellent with minimal discomfort in the surgery area and with minimal postoperative inflammation.
Figures 2-19 show one of the cases included in the study.
Transcrestal sinus lift with short and extra-short implants is a highly predictable technique with high success rates for elevated implant, finding slight differences in residual bone volume. The survival of short and extra-short implants inserted by a transcrestal procedure when residual bone crest is 5 mm high or more is found in 94.9%, compared to 92.7% reported for cases where these implants are inserted in areas with severe vertical resorption (less than 5 mm of residual bone height)21,22. This decrease in predictability may be due to the milling sequence, stabilization of the implant and the surface of the implant, since they are elements that play in favour of achieving a primary stability in areas with low density and this can make the difference in limit cases13,24,27,30-33. In implant insertion surgery, we can modify all the parameters except bone density to play in our favour and achieve greater primary stability in cases where the bone does not offer a correct stability by itself. It is possible to vary the implant to use, its diameter and in many cases its length (extra-short implants 4.5-5-5 mm), as well as adapt the milling sequence to achieve compression.
In addition, the use of bioactive implant surfaces, which accelerate bone formation in contact with the graft substrate can lead to substantial improvement of the
results obtained when increasing the height of bone volume above the apex as well as the posterior maintenance. The load received by the implant is also key in maintaining the increased bone. A poor design of the prosthesis can result in the best surgeries not being successful. Therefore, the work of prostheses on transepithelial instead of directly to implant, the maintenance of implant-prosthesis hermeticity and the distancing of the critical attachment area of the implant with the prosthesis (with the height of the transepithelial next to or slightly supra-gingival areas) it can make the success achieved in the first phase of the treatment to be retained after loading24-25.
To achieve the success of the implants placed in areas of extreme horizontal atrophy by a transcrestal sinus approach with extra-short implants is possible, provided that a correct stabilization of the implant is achieved in the initial phase (primary stability) and a careful milling protocol is used, insertion of the implant, management of the graft, 100% processing of bone and autologous plasma and subsequent loading of the same (progressive loading).
Pommer B, Mailath-Pokorny G, Haas R, Busenlechner D, Fürhauser R, Watzek G. Patients‘ preferences towards minimally invasive treatment alternatives for implant rehabilitation of edentulous jaws. J Oral Implantol 2014;7(2: -109 -109.
Lin Z, He B, Chen J, D u Z, Zheng J, Li Y. [Manufacture method and clinical application of minimally invasive dental implant guide template based on registration technology]. Hua Xi Kou Qiang Yi Xue Za Zhi 2012;30:402-6, 410.
Azar DE. Minimally Invasive Single- Implant Treatment in the Esthetic Zone. Compend Contin Educ Dent 2017;38:241-7.
Al-Hashedi AA, Taiyeb Ali TB, Yunus N. Short dental implants: an emerging concept in implant treatment. Quintessence Int 2014;45:499-514.
Altaib FH, Alqutaibi AY, Al-Fahd A, Eid S. Short dental implant as alternative to long implant with bone augmentation of the atrophic posterior ridge: a systematic review and meta-analysis of RCTs. Quintessence Int 2019;50:636-50.
Malchiodi L, Ricciardi G, Salandini A, Caricasulo R, Cucchi A, Ghensi
P. Influence of crown-implant ratio on implant success rate of ultra-short dental implants: results of a 8- to 10-year retrospective study. Clin Oral Investig 2020;24:3213-22.
Anitua E, Alkhraisat MH. 15-year follow-up of short dental implants placed in the partially edentulous patient: Mandible Vs maxilla. Ann Anat 2019;222:88-93.
Anitua E, Orive G, Aguirre JJ, Andía I. Five-year clinical evaluation of short dental implants placed in posterior areas: a retrospective study. J Periodontol 2008;79:42-8.
Stern A, Green J. Sinus lift procedures: an overview of current techniques. Dent Clin North Am 2012;56:219-33.
Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium 1994;15:152-62.
Kühl S, Kirmeier R, Platzer S, Bianco N, Jakse N, Payer M. Transcrestal maxillary sinus augmentation: Summers‘ versus a piezoelectric technique–an experimental cadaver study. Clin Oral Implants Res 2016;27:126-9.
Anitua E, Flores J, Alkhraisat MH. Transcrestal sinus floor augmentation by sequential drilling and the use of plasma rich in growth factors. Int J Oral Maxillofac Implants 2017;32:e167–e173.
Blase DV, Dricot RG, Lasserre JF, Toma S, Brecx MC. Combination of a hydraulic device and nanohydroxylapatite paste for minimally invasive transcrestal sinus floor elevation: Procedure and 4-year results. Int J Oral Maxillofac Implants 2021;36:587-597.
Wang H, Wang J, Guo T, et al. The endoscopically assisted transcrestal sinus floor elevation with platelet-rich fibrin at an immediate implantation of periapical lesion site: A case report. Medicine (Baltimore) 2019;98:e16251.
Cho YS, Hwang KG, Jun SH, Tallarico M, Kwon AM, Park CJ. Radiologic comparative analysis between saline and platelet-rich fibrin filling after hydraulic transcrestal sinus lifting without adjunctive bone graft: A randomized controlled trial. Clin Oral Implants Res 2020;31:1087-1093.
Kappel S. The effect of transcrestal sinus-floor elevation without graft on the long-term prognosis of maxillary implants. J Clin Periodontol. 2020;47:640-648.
Therapeutic outcomes of non- grafted and platelet concentrations- grafted transcrestal maxillary sinus elevation (TSFE): a systematic review and meta-analysis. Sci Rep 2020;10:5935.
Anitua E, Flores J, Alkhraisat MH. Transcrestal sinus lift using platelet concentrates in association to short implant placement: A retrospective study of augmented bone height remodeling. Clin Implant Dent Relat Res 2016;18:993-1002.
Del Fabbro M, Corbella S, Weinstein T, Ceresoli V, Taschieri S. Implant survival rates after osteotome-mediated maxillary sinus augmentation: a systematic review. Clin Implant Dent Relat Res 2012; 14(Suppl 1):e159–e168.
E. Soardi, F. Cosci, V. Checchi, G. Pellegrino, P. Bozzoli, and P. Felice, “Radiographic analysis of a transalveolar sinus-lift technique: a multipractice retrospective study with a mean follow-up of 5 years,” J Periodontol 2013;84:1039–1047.
M. Del Fabbro, S. Corbella, T. Weinstein, V. Ceresoli, and S. Taschieri, “Implant survival rates after osteotome-mediated maxillary sinus augmentation: a systematic review,” Clinical Implant Dentistry and Related Research 2012;14, supplement 1:e159–e168.
Anitua E, Alkhraist MH, Piñas L, Orive G. Association of transalveolar sinus floor elevation, platelet rich plasma, and short implants for the treatment of atrophied posterior maxilla. Clin Oral Implants Res 2015; 26:69–76.
Franceschetti G, Farina R, Minenna L, et al. The impact of graft remodeling on peri-implant bone support at implants placed concomitantly with transcrestal sinus floor elevation: A multicenter, retrospective case series. Clin Oral Implants Res 2020;31:105-20.
Lo Giudice G, Iannello G, Terranova A, Lo Giudice R, Pantaleo G, Cicciù
M. Transcrestal sinus lift procedure approaching atrophic maxillary ridge: A 60-month clinical and radiological follow-up Evaluation. Int J Dent 2015;2015:261652.
Anitua E, Piñas L, Alkhraisat MH. Early marginal bone stability of dental implants placed in a transalveolarly augmented maxillary sinus: a controlled retrospective study of surface modification with calcium ions. Int J Implant Dent 2017;3:49.
Anitua E, Cerqueira A, Romero- Gavilán F, García-Arnáez I, Martinez-Ramos C, Ozturan S, Azkargorta M, Elortza F, Gurruchaga M, Goñi I, Suay J, Tejero R. Influence of calcium ion-modified implant surfaces in protein adsorption and implant integration. Int J Implant Dent 2021;7(1):32.
Anitua E, Prado R, Orive G. A lateral approach for sinus elevation using PRGF technology. Clin Implant Dent Relat Res 2009;11 Suppl 1:e23-31.
Anitua E, Piñas L, Murias A, Prado R, Tejero R. Effects of calcium ions on titanium surfaces for bone regeneration. Colloids Surf B Biointerfaces 2015;130:173-81.
Anitua E, Prado R, Orive G, Tejero R. Effects of calcium-modified titanium implant surfaces on platelet activation, clot formation, and osseointegration. J Biomed Mater Res A 2015;103:969-80.
Anitua E, Alkhraisat MH, Pinas L, Orive G. Efficacy of biologically guided implant site preparation to obtain adequate primary implant stability. Ann Anat 2015;199:9–15.
Lee H, Jo M, Sailer I, Noh G. Effects of implant diameter, implant- abutment connection type, and bone density on the biomechanical stability of implant components and bone: A finite element analysis study. J Prosthet Dent 2021 5:S0022- 3913(20)30655-7.
Hernández-Marcos G, Hernández- Herrera M, Anitua E. Marginal bone loss around short dental implants restored at implant level and with transmucosal abutment: A Retrospective Study. Int J Oral Maxillofac Implants 2018;33:1362-7.
Anitua E, Alkhraist MH, Piñas L, Begoña L, Orive G. Implant survival and crestal bone loss around extra- short implants supporting a fixed denture: the effect of crown height space, crown-to-implant ratio, and offset placement of the prosthesis. Int J Oral Maxillofac Implants 2014;29:682-9.

Anitua, Eduardo
DDS, MD, PhD.
Private practice in oral implantology, Eduardo Anitua Clinic Vitoria, Spain. University Institute for Regenerative Medicine and Oral Implantology – UIRMI (UPV/ EHU) Eduardo Anitua Foundation),
Vitoria, Spain. BTI Biotechnology institute (BTI), Vitoria, Spain.