Clinical case
Published in spanish Científica Dental Vol. 17. Nº 2. 2020 www.cientificadental.es
Digital flow in unitary dental implants rehabilitation in anterior sector. Surgical and prosthetic planning. Case report
Aim: The purpose of this article is to present a clinical case of high aesthetic demand. Such planning and treat with digital flow, included diagnosis, prosthetic planning and finally, the placement of the final prosthesis.
Case report: A 52-year-old woman presents a fracture of the tooth 2.1. After diagnosis and analysis both clinically and radiographically, an impossible restorative prognosis is determined for 2.1, planning implant-supported rehabilitation as treatment. A scan of the area to be treated was carried out to carry out a detailed study of the case and the preparation of a provisional crown, which was screwed at the same time of surgery to an implant placed immediately post-extraction. Besides, hard and soft tissue graft were placed to guarantee the maintenance of the peri-implant contours. After the implant osteointegration, the contour of the provisional crown was scanned to obtain a suitable emergence profile and gingival tissue volume. Both the emergency profile obtained and the contour of the provisional were scanned together with the position of the implant for the preparation of the final metalceramic restoration. After six months, it can observe an ideal soft tissue aesthetic and perfect maintenance of the entire gingival architecture.
Conclusion: The management of the anterior superior aesthetic sector shows a clear aesthetic demand. In cases of tooth loss at this location, fixed implant rehabilitation is the treatment of choice. However, to achieve an adequate and predictable result, proper surgical and prosthetic management is essential. Digital flow it present like alternative and a quality leap in the therapeutic approach to these cases, a more accurate and individualized treatment, and the information that is transferred to the prosthetic laboratory is more simple and efficient.
After the loss of a tooth, a series of physiological processes takes place throughout the dento-alveolar complex that culminates in atrophy and collapse of both the bone and gum tissues, with a horizontal and vertical component. This can have a significant repercussion aesthetically for patients when it affects the anterosuperior aesthetic sector1-. Following advances in rehabilitation of osseointegrated implants (OII), aimed at achieving greater primary stability in post-extraction sockets and allowing a reduction in integration times, new treatment protocols have emerged that can focus rehabilitation on aesthetic sectors much more efficiently. These protocols are based mainly on immediate placement of the screw-retained provisional crowns at the same time during surgery. This allows for the preservation and management of soft and hard tissue grafts and emergency profiles; thus preventing their collapse and giving the patient immediate aesthetic benefit4-6.
Nowadays, digital workflow is increasingly integrating itself in practically all dentistry fields, although its application in oral rehabilitation and cosmetic dentistry is especially important. Implants can be planned following advances in technologies and the use of intraoral scanners and software programs. These digital programs can be used to design the case by computer, analyse the patient photographic study and make virtual study models to improve case planning; thus reducing treatment times and, in the long run, their costs, with respect to traditional methods7, 8.
Digital planning as part of implant rehabilitation is a tool for optimising results and improving surgical planning, which is prosthetically guided from the outset and can lead to more exact handling of peri-implant tissues, thanks to scanning the emergence profiles obtained, and making definitive restorations of great aesthetic quality7, 8.
The objective of this article is to describe the rehabilitation on implants in a high aesthetic demand case, with the treatment based entirely on digital planning.
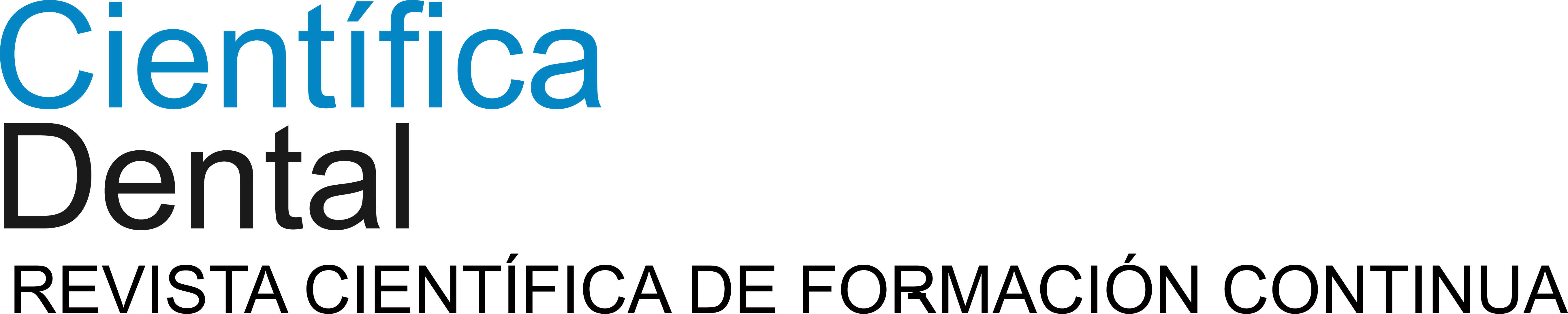
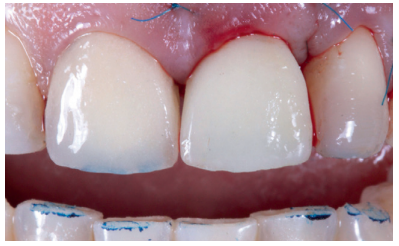
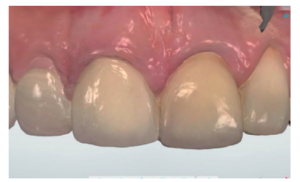
This describes the clinical case of a 52-year-old woman who came to the dentist surgery due to de-cementation of a tooth-supported metal-ceramic crown on tooth 2.1 (ICSI), see Figures 1-3. The patient reported it as of high concern for her aesthetically.


She had no notable medical, personal or surgical history, and reported not being a habitual smoker or drinker, and was therefore an ASA class I patient.
Examination
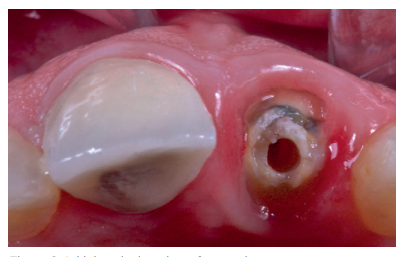
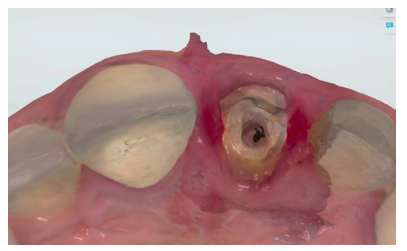
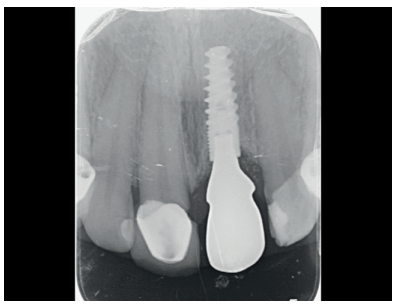
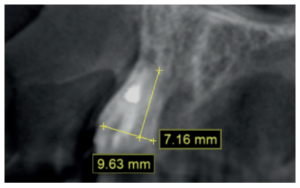
The patient reported pain when chewing in the anterosuperior sector, located in the ICSI area, which disappeared after taking painkillers. An intraoral clinical examination revealed that the decemented crown retained remains of the ICSI stump, as well as a cast post that served as a scaffold for the restoration. The ICSI was a root remnant, with total loss of tooth structure and no ferrule that might ensure a new rehabilitation9 . The patient had a medium smile line and a fine gingival phenotype, which was accompanied by gingival recession in the affected tooth, as well as in the contiguous teeth of the second quadrant. She presented palpation, percussion and a positive bite test and negative vitality in the ICSI, with no periodontal pocket (probe depth < 3 mm) or mobility. An additional radiological examination was carried out, which included a periapical radiograph and cone beam computed tomography (CBCT), see Figure 4. After evaluating these tests, a subgingival complete horizontal coronary fracture without periapical bone involvement was observed.
Diagnosis and treatment plan
Following the examination and the additional tests, restoring the ICSI was considered impossible. Due to the clinical features of the case, and with the agreement of the patient, the treatment plan was to extract the ICSI and insert an osseointegrated implant (OII), associated with a provisional implant-retained prosthesis at the same time. The apical residual bone was favourable for inserting the OII, as it was a Class I socket according to Kan10, and with practically total integrity of the vestibular surface, being a type I socket according to Elian11.
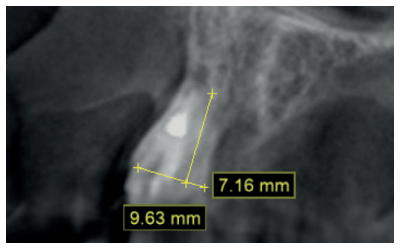
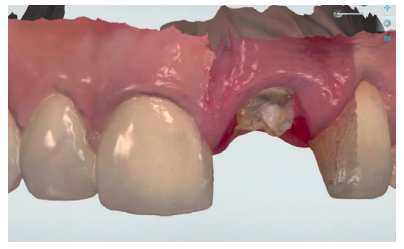
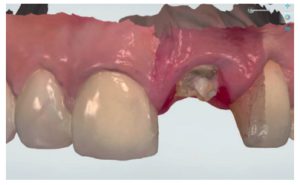
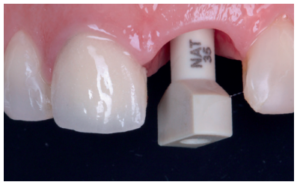
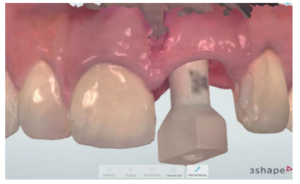
Using a 3Shape™ scanner, an intraoral pre-scan was performed, first with the tooth-supported crown in place, to obtain the anatomy of the central incisor, and then without it; thus scanning the emergence profile of the root rest; the laboratory was informed of the modification of the critical profile, thus correcting the existing recession with respect to 1.1 (Figures 5-7). This scan served in turn to take the colour of the future provisional structure7, 8. The STL file was sent to the laboratory to make the Marylandtype provisional prosthesis, in polymethyl methacrylate (PMMA), with two supports on the incisor edges of the adjacent teeth to ensure their correct positioning. According to the plan performed beforehand, this would serve as a provisional tooth, as well as surgical guide for the insertion of the OII in the ideal prosthetic position; thus avoiding possible future problems at the prosthetic level or in the integrity of the soft and hard tissues of the vestibular region (Figures 8 and 9).
Surgical approach
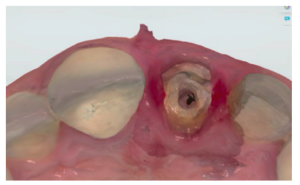
After anaesthetic infiltration (4% articaine with 1: 100,000 adrenaline), the root of the affected tooth was extracted. As a complication of the extraction, the distal papilla was lacerated, which was repaired with a single stitch. The residual socket was then evaluated to prepare the bed to insert the OII. This was intact, with intact vestibular cortex.
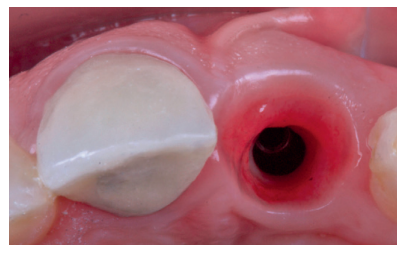
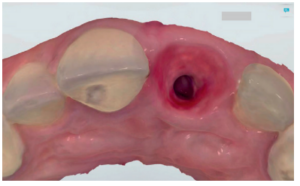
The OII (ETK-Naturactis™, 4 x 12 mm) was placed at a depth of 4 mm with respect to the future gingival margin that needed to be achieved. The margin of the provisional prosthesis was used as a reference, similar to the gingival margin of the adjacent central incisor that was maintained without recession.
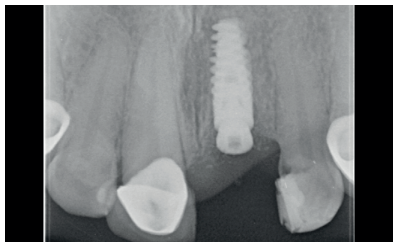
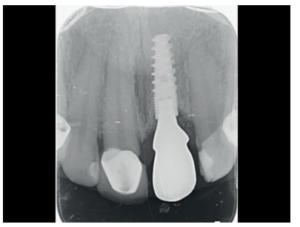
Proper primary stability was obtained, with anchorage achieved in the residual palatal bone at an insertion torque of 40 N/cm2 . A periapical radiograph was performed to confirm the position (Figure 10).

Provisional prosthetic phase
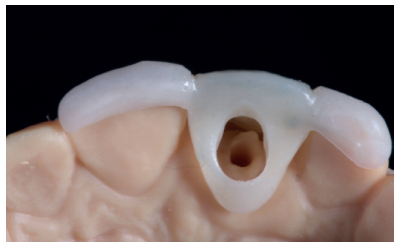
Before starting the provisional restoration screwed onto the OII, its disposition with respect to the metal abutment, the mesio-distal adaptation and the contact points to the adjacent teeth were all verified as correct, and the absence of compression on the interdental papillae was ensured. The critical contour of the provisional was designed at the same level as the gingival margin of the adjacent central incisor crown, which was considered ideal, thanks to the photos and the previous pre-scan, leaving 1.5 mm supragingival, due to the previous recession. The abutment was relined with the provisional using 3M™12 flowable composite. Next, the subcritical profile was prepared, by providing a concave contour to allow space for the formation of connective tissue. Finally, it was verified that the provisional was completely polished over its entire surface13.
Hard and soft tissue management
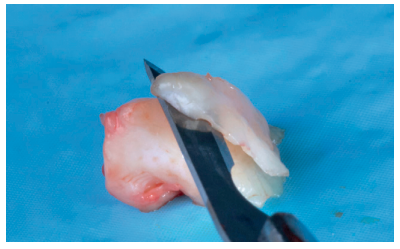
In these types of cases, the management of hard and soft tissue is of special importance. Due to the thin gingival phenotype, the collapse of the vestibular soft tissue, always associated with an extraction, and the pre-existing recession, a tuberous connective tissue graft (CTG) was performed using the envelope technique (Figure 11)14,15.
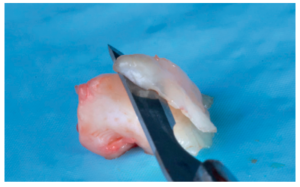
The CTG was adapted to the recipient region using a 6.0 monofilament suture. Subsequently, the gap in the vestibular region of the alveolus was filled to minimise its collapse. For this, autologous bone collected from drilling was used in the area near the OII and xenograft in the most vestibular area (OsteoBiol™ Apatos)16.
To complete the surgical approach, the provisional prosthesis was screwed in, and its complete anocclusion checked, both for maximum intercuspation and eccentric movements, using articulating paper (Figure 12). The patient was instructed to avoid any type of functional load on the provisional during the entire osseointegration time of the implant. Antibiotic treatment was prescribed, with amoxicillin/clavulanic acid, 500/125mg, 1 tablet every 8 hours for 7 days, as well as a painkiller regimen, with prescription of dexketoprofen 25mg, with the same dosage as the antibiotic.
The patient returned 7 days later for a check-up; good healing of the peri-implant tissues was observed (Figure 13). Another week later, 14 days after surgery, the suture was removed. The patient attended monthly check-up appointments until the end of the osseointegration time.

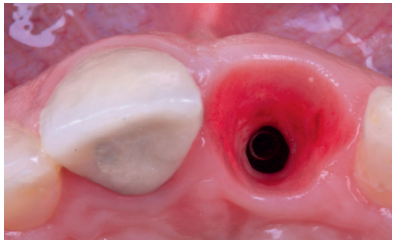
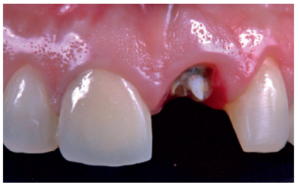
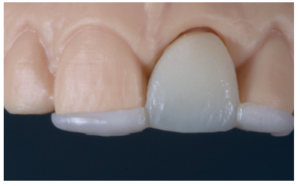
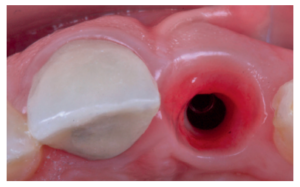
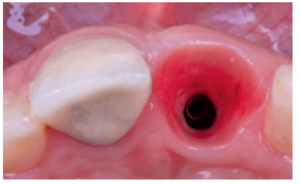
Soft tissue management with the provisional crown
The provisional was removed after 14 weeks, when the gingival margin was seen to be correctly positioned, along with 100% coverage of the recession, complete papillae maintenance and a correct emergence profile (Figures 14 and 15). However, from an occlusion view, there was a lack of buccal volume with respect to the adjacent tooth. Work began with the provisional crown, with progressive increases of composite in the subcritical profile, until a volume similar to tooth 1.1 was achieved. These increases were performed every 15 days (Figure 16)13.

Final measurements
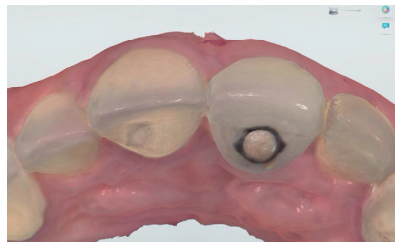
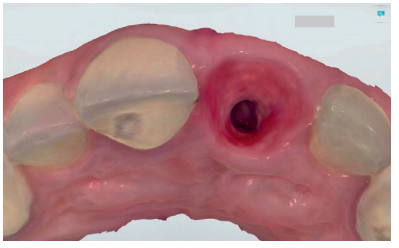
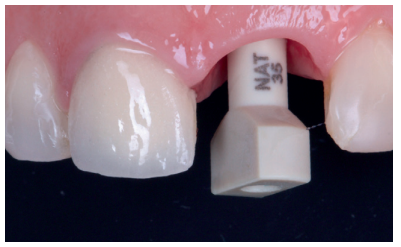
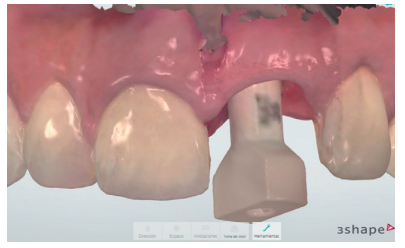
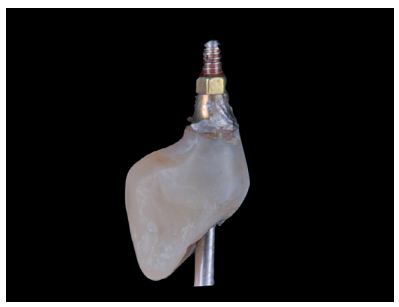
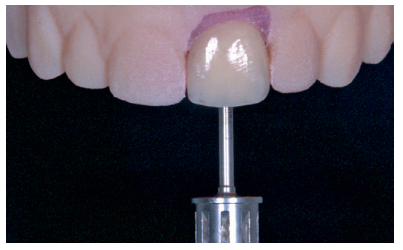
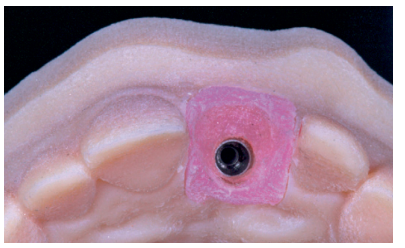
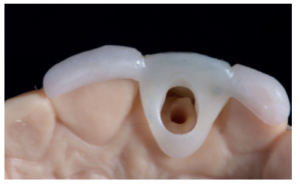
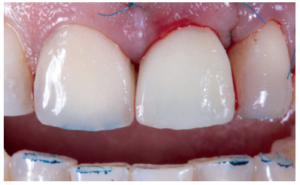
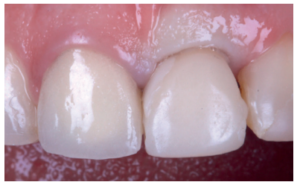
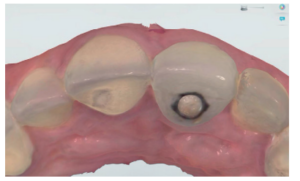
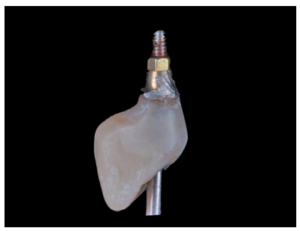
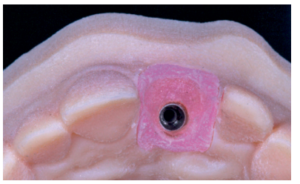
After achieving optimal tissue volume by handling the provisional (Figure 17), an initial scan of the maxilla was performed with the screw-retained provisional crown to obtain the anatomy (Figure 18). Subsequently, a second scan was performed without it, with accurate recording of the gingival contours and the emergence profile achieved (Figure 19), as well as the implant position using the scan body (Figures 20 and 21). For proper recording of the emergence profile, the provisional crown was scanned outside the mouth (Figures 22 and 23); thus avoiding having to perform the classic technique of an individualised transfer17. These records were sent to the prosthetic laboratory, which designed a post-machined sintered metal structure (Figure 24). Once the framework test had been satisfactorily carried out (Figure 25), the colour of the restoration (A2 VITA guide) was taken using a polarised light filter (Figure 26). These records were sent back to the prosthetic laboratory for completion of the implant-retained crown on the printed models (Figures 27 and 28). Prior to the placement of the definitive crown, the emergence profile of the provisional crown was compared with the final one, and the similarity observed between them (Figure 29); thus managing to preserve the profiles maintained from the day treatment was started.





After the 6-month review, excellent stability of all periimplant tissues was verified, with correct volume at the vestibular level, as well as the maintenance of optimal aesthetics and functionality (Figure 30).

In recent years, implantology has undergone a series of advances that have gone hand in hand with technology. At the beginning of this field of dentistry, placing an implant in a post-extraction socket was not conceivable, in the same way that the implant load was not evaluated in the same surgical act. However, this initial, classic vision18, 19 has turned towards treatments where prosthetic rehabilitation takes on special importance, as well as for the time in which it occurs. Scientific endorsement of the new techniques is also supporting the use of digital resources20, 21. These resources in implantology have improved diagnosis and allowed for the establishment of more reliable treatment plans. The standardisation and quality of these procedures has increased in recent years, offering the patient a higher quality of treatment in a shorter time. Thus, digital workflow in dentistry has proven to be more efficient than the conventional working method in terms of cost and time, as well being better accepted by patients. Taking digital impressions allows for a better recording of occlusion and greatly reduces the distortions present in analogue procedures. As well as the use of photographic analysis, the different design software programs and the study of models at a digital level, this all means that dental prosthetic rehabilitation therapies are carried out with greater safety and quality20-23.
Different studies have shown that there is a higher risk of failure in single implants subjected to immediate loading compared to multiple restorations, even with a high insertion torque. Therefore, the concept of “loading” has changed to that of “provisionalisation”, since the provisional crown is completely exempt from function. The importance of these provisional restorations, in addition to immediate aesthetics, lies in the maintenance of the gingival contour and the interdental papillae; favouring the maintenance of volume and reducing horizontal and vertical collapse due to tooth loss4-6, 24.
The implementation of intraoral scanning and digital flow in implant restorations of high aesthetic demand allows for the creation of more accurate provisional restorations due to greater precision in the analysis of the case. From study of the software, soft tissue status can be determined and provisionals developed according to individual needs to obtain optimal gingival contours and volume. Likewise, pre-scanning the provisional restorations means that the subcritical contour the final crown must have can be transferred to the laboratory, faithfully and almost exactly; ensuring the maintenance of the gingival morphology and the long-term success of the case25,26. In this instance, a surgical guide to perform guided surgery was not manufactured, since the provisional rehabilitation itself was used as a guide, using support on the incisor edges and in the palatal region, thus simplifying the treatment complexity. Proper design of the provisional prosthesis, its digital scanning and scanning of the emergence profiles make it possible to shorten the times and the number of tests to perform the final prosthesis23.
Management of the anterior superior aesthetic sector shows a clear aesthetic requirement. In cases of tooth loss in this location, fixed rehabilitation on implants is the treatment of choice. However, to achieve an adequate, reliable result, proper surgical and prosthetic management is essential. Digital planning represents a leap in quality in the therapeutic approach to these cases, providing more exact, individualised and reliable treatment, with the information transferred to the prosthetic laboratory being simpler and more efficient.
Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol 2005; 32 (2): 212-8.
Araújo MG, Sukekava F, Wennström JL, Lindhe J. Ridge alterations following implant placement in fresh extraction sockets: an experimental study in the dog. J Clin Periodontol 2005; 32 (6): 645-52.
Araújo MG, da Silva JCC, de Mendonça AF, Lindhe J. Ridge alterations following grafting of fresh extraction sockets in man. A randomized clinical trial. Clin Oral Implants Res 2015; 26 (4): 407-412.
Higginbottom F, Belser R, D. Jones J, E. Keith S. Prosthetic management of implants the esthetic zone. Int J Oral Maxillofac Implants 2004; 19: 62-72.
Al-Sabbagh M. Implants in the Esthetic Zone. Dent Clin North Am 2006; 50: 391–407.
Buser et al. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants 2004; 19: 43-61.
Joda T, Brägger U, Gallucci G. Systematic literature review of digital threedimensional superimposition techniques to create virtual dental patients. Int J Oral Maxillofac Implants 2015; 30: 330-7.
Stapleton BM, Lin WS, Ntounis A, Harris BT, Morton D. Application of digital diagnostic impression, virtual planning, and computer-guided implant surgery for a CAD/CAM-fabricated, implant-supported fixed dental prosthesis: a clinical report. J Prosthet Dent 2014; 112: 402-8.
Santos D, Valenzuela F, Morrow B, Pameijer C, Garcia-Godoy F.Effect of Ferrule Location With Varying Heights on Fracture Resistance and Failure Mode of Restored Endodontically Treated Maxillary Incisors. J Prosthodont 2019; 28 (6): 677-683.
Kan JY, Roe P, Rungcharassaeng K, Patel RD, Waki T, Lozada JL, Zimmerman G. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: a cone beam computed tomography study. Int J Oral Maxillofac Implants 2011; 26 (4): 873-6.
Elian N, Cho SC, Froum S, Smith RB, Tarnow DP. A simplified socket classification and repair technique. Pract Proced Aesthet Dent 2007; 19 (2): 99-104.
Gallucci G,Bernard J, Med P, Bertosa M, Berlser U. Immediate Loading with Fixed Scre-Retained Provisional Restorations in Edentulous Jaws: The Pickup Technique. Int J Oral Maxillofac Implants 2004; 19: 524-533.
Su H, Gonzalez-Martin O, Weisgold A, Lee E. Considerations of implant abutment and crown contour: critical contour and subcritical contour. Int J Periodontics Restorative Dent 2010; 30 (4): 335-43.
Fu JH, Lee A, Wang HL. Influence of tissue biotype on implant esthetics. Int J Oral Maxillofac Implants 2011; 26 (3): 499-508.
Tatakis DN, Chambrone L, Allen EP y cols. Periodontal soft tissue root coverage procedures: a consensus report from the AAP Regeneration Workshop. J Periodontol 2000 2016; 86 (2 Suppl): S52-5.
Sanz M, Lindhe J, Alcaraz J, Sanz-Sanchez I, Cecchinato D. The effect of placing a bone replacement graft in the gap at immediately placed implants: a randomized clinical trial. Clin Oral Impl Res 2016; 28: 1-9.
Hinds KF. Custom impression coping for an exact registration of the healed tissue in the esthetic implant restoration. Int J Periodontics Restorative Dent 1997 Dec; 17(6): 584-91.
Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981; 10: 387-416.
Brånemark PI. Osseointegration and its experimental background. J Prosthet Dent 1983; 50: 399-410.
Joda T, Brägger U. Digital vs. conventional implant prosthetic workflows: a cost/ time analysis. Clin Oral Impl Res 2015; 26: 1430-5.
Pacifici L, Pacifici A. Digital flow in medicine and dentistry: what’s new? J Biol Regul Homeost Agents 2018; 32 (4): 1027- 1031.
Wismeijer D, Mans R, van Genuchten M, Reijers HA. Patients’ preferences when comparing analogue implant impressions using a polyether impression material versus digital impressions (Intraoral Scan) of dental implants. Clin Oral Implants Res 2014; 25: 1113-8.
Joda T, Brägger U. Patient-centered outcomes comparing digital and conventional implant impression procedures: a randomized crossover trial. Clin Oral Implants Res 2016; 27(12): e185-e189.
Buser D, Chappuis V, Belser UC, Chen S. Implant placement post extraction in esthetic single tooth sites: when immediate, when early, when late? Periodontol 2000 2017; 73 (1): 84-102.
Joda T, Gallucci GO. The virtual patient in dental medicine. Clin Oral Implants Res 2015; 26: 725-6.
Arunyanak SP, Harris BT, Grant GT, Morton D, Lin WS. Digital approach to planning computer-guided surgery and immediate provisionalization in a partially edentulous patient. J Prosthet Dent 2016; 116: 8-14.

Moreno Pérez, Natalia
Private practice, Madrid.
Peña Cardelles, Juan Francisco
Professor for Master’s in Oral Surgery and Implantology, Rey Juan Carlos University, Madrid. Collaborating professor in the Master’s of Prosthetics on Implants, Rey Juan Carlos University.
Otero Mena, Isabel
Professor in the Master’s of Oral Surgery and Implantology, Rey Juan Carlos University, Madrid. Private practice, Madrid.
Ortega Concepción, Daniel
Professor in the Master’s of Oral Surgery and Implantology, Rey Juan Carlos University, Madrid. Collaborating professor in the Master’s of Prosthetics on Implants, Rey Juan Carlos University.
Moreno Pérez, Jesús
Private practice, Madrid. Collaborator in the Master’s in Oral Surgery and Implantology, Rey Juan Carlos University, Madrid.