Case report
Published in spanish Científica Dental Vol. 21. Nº 2. 2024
www.cientificadental.es
Surgical and restorative management of a dental implant in the esthetic zone and volumetric evaluation following deepithelialized connective tissue graft: a case report
Introduction (basis and objectives): After tooth extraction, changes occur in the soft tissues associated with bone resorption in a vertical and horizontal direction. This collapse can be addressed through bone grafts and connective tissue grafts. The objective of this clinical case is to describe the treatment sequence carried out from extraction to delivery of the definitive crown, combining regenerative, guided surgery, mucogingival and prosthetic concepts. Furthermore, changes in vestibular mucosal thickness that occurred after the use of a connective tissue graft are described and analyzed using digital analysis software.
Methods: The surgical sequence consisted of performing alveolar preservation. After 4 months, a guided implant was planned and placed in position 1.2 with simultaneous connective tissue graft. After integration, the soft tissues were conditioned with a provisional crown and then the definitive screw-retained restoration was placed.
Results: The guided implant placement approach and application of a connective tissue graft showed aesthetic results and significant soft tissue volumetric gains.
Conclusions: Careful management of hard and soft tissues, as well as planning through guided surgery, increases precision regarding the ideal position of the implant, which will impact the long-term stability of hard and soft tissues.
Key words: Surgery; Computer-Assisted; Dental implants; Soft tissue; Connective tissue; Software tool.
In the field of implantology, digital technology has emerged as an advancement to enhance surgical procedures and achieve high-quality treatments with aesthetic outcomes. In this context, guided surgery, introduced in the 1990s, is regarded as a contemporary dental practice based on digital planning and the utilisation of advanced imaging technologies1. Implant placement is performed using 3D-printed surgical guides and a specific kit designed for each system2. Compared with the conventional technique, guided implant placement has been demonstrated to significantly optimise safety, minimise injury to adjacent anatomical structures, and reduce surgical time as well as intra- and postoperative morbidity3–5. However, guided surgery requires a financial investment, more meticulous advance planning, and a professional with broader experience for its appropriate management2,6.
There is no doubt that the aesthetic outcome of treatment with implants in the anterior maxillary region is of great importance. For this purpose, it is essential to have adequate peri-implant tissue support, encompassing both hard and soft tissues. Each professional must assume responsibility for improving the phenotype of peri-implant soft tissues, focusing on three main components: gingival thickness, width of keratinised mucosa, and supracrestal tissue height7,8. Current research recognises soft tissue augmentation procedures as essential interventions. They not only enhance stability at the bone level but also control inflammatory signs and prevent future aesthetic complications7,9–11.
Over the past decade, the quantitative evaluation of augmented tissues has primarily relied on clinical methods such as the periodontal probe and endodontic files. However, the analogue instruments employed lack three-dimensional accuracy for the precise assessment of volumetric changes12. Consequently, the utilisation of digital technologies such as computed tomography, ultrasound, and three-dimensional analysis of STL (Standard Tessellation Language) files derived from the digitisation of plaster models or intraoral scanning is advantageous13–15. These digital and computerised tools offer significant advantages in dental diagnosis, planning, and treatment. Thus, they provide non-invasive and comfortable measurements for patients, greater accuracy in 2D and 3D evaluations (achieving a precision of 0.01 mm), and enable long-term monitoring by analysing changes occurring in the tissues16,17.
The objective of this clinical case is to present a treatment sequence in a clinical scenario where anatomical and restorative conditions precluded the placement of an immediate implant in the aesthetic sector. Furthermore, to describe and evaluate, using a non-invasive technique and three-dimensional analysis software, the volumetric changes of the soft tissue following the placement of a connective tissue graft on the buccal and occlusal aspects of the implant.
1.1 Diagnosis and Treatment Plan
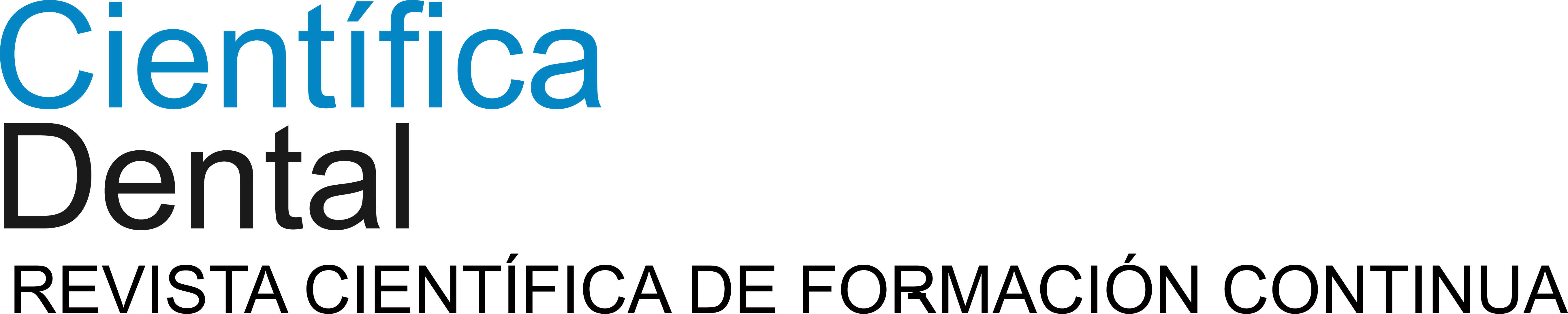
A 29-year-old female patient presented to our dental clinic following trauma to the right maxillary lateral incisor (1.2). The trauma resulted in a fracture of the entire anatomical crown; consequently, only a root remnant in a subgingival position remained. The root remnant was diagnosed as non-restorable, and the available therapeutic options were thoroughly discussed with the patient. It was decided to replace tooth 1.2 with a dental implant, and the following treatment plan and clinical sequence were established: Phase I: extraction of the root remnant 1.2 and reconstruction of the alveolar process using a minimally invasive alveolar preservation procedure.
Immediate provisional restoration using a removable partial acrylic prosthesis. Phase II: guided placement of an implant and augmentation of mucosal thickness with a connective tissue graft. Phase III: shaping and modelling
of the emergence profile using a direct implant provisional prosthesis and definitive ceramic implant restoration.
1.2 Treatment
• Phase I: atraumatic extraction of the root remnant 1.2 was performed, followed by curettage of the granulation tissue. Subsequently, the alveolus was filled with an inorganic bovine bone graft (0.25–1mm) combined with autologous platelet- and leukocyte-rich fibrin. Finally, the edges were approximated and sutured with four simple stitches from the vestibular mucosal margin to the palatal aspect. Subsequently, the patient continued using her removable partial denture as a provisional restoration (Figure 1).
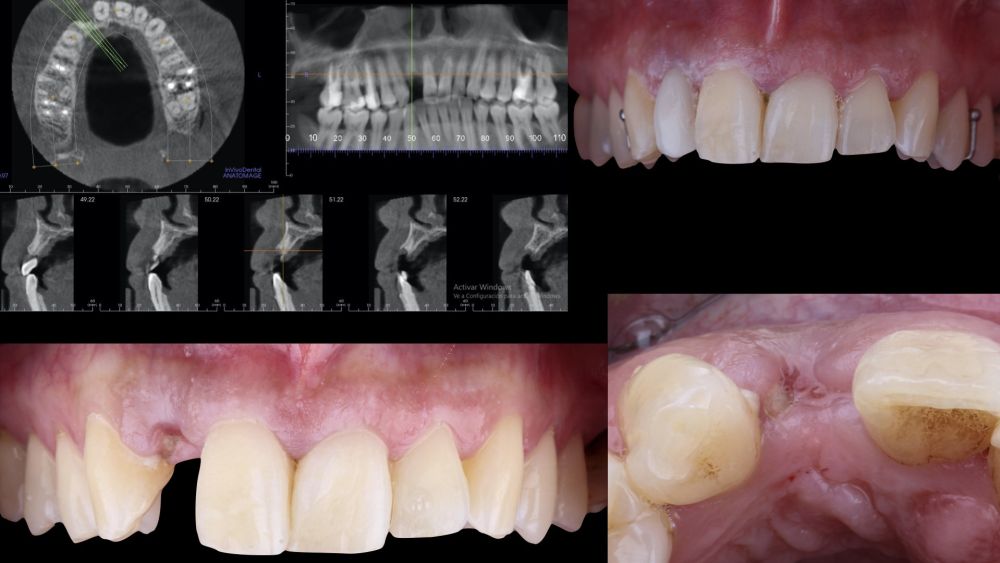
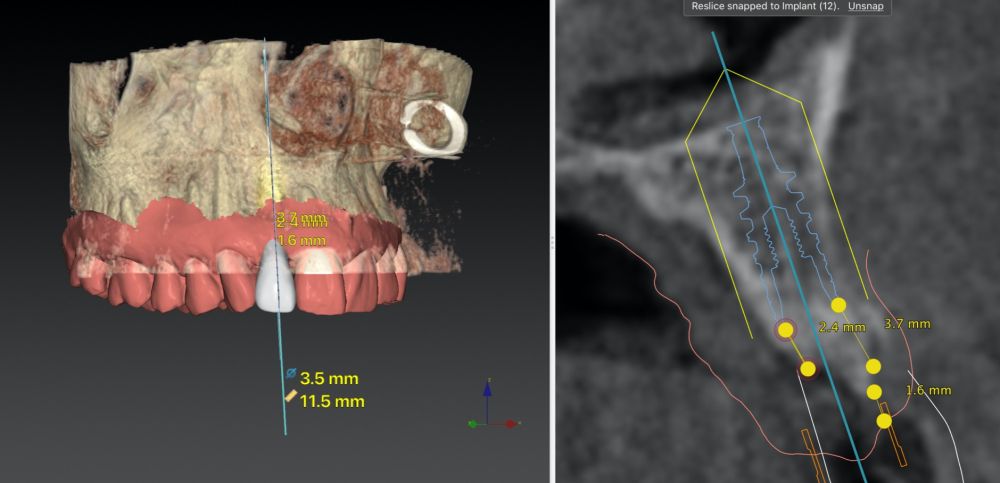
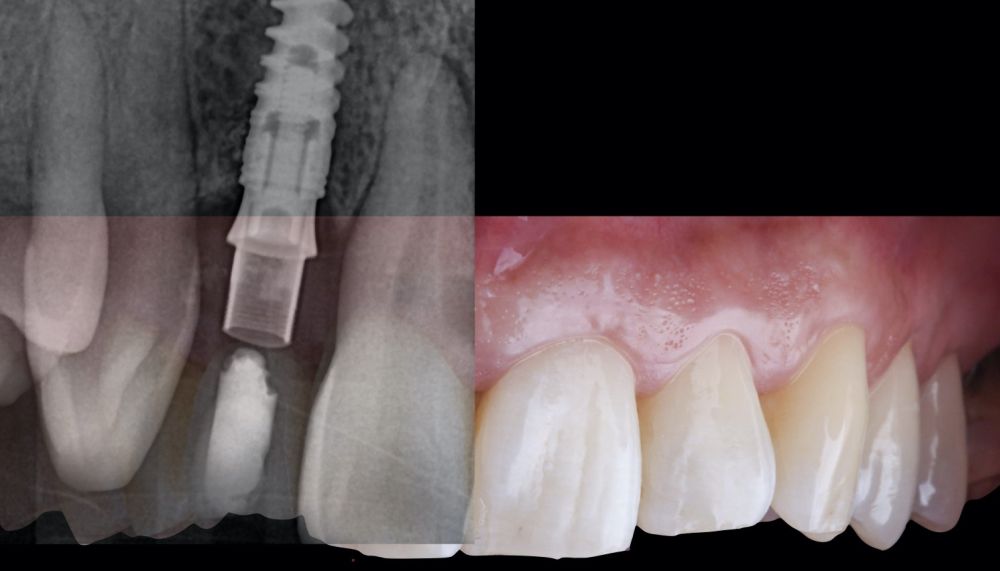
* Phase II: healing proceeded without complications. After 5 months from the alveolar preservation surgery, guided implant surgery was planned at position 1.2 (Figure 2). For this purpose, a DICOM file from cone beam computed tomography (CBCT) and an STL file obtained from scanning with an intraoral optical scanner were used. Using this information, a dental support surgical guide was fabricated (Figure 3). The surgical guide was anchored onto the teeth and guided the preparation of the implant bed and the placement of the implant. The guided surgery technique consisted of flap surgery, preparing and inserting the implant (3.5 x 11.5 mm) according to the standardised Nobel Active® guided surgery protocol (Nobel Biocare AB, Gothenburg, Sweden). Once implant 1.2 was placed,a gingival graft composed of epithelium and connective tissue from the palatal masticatory mucosa was obtained. Subsequently, the superficial epithelial layer of this graft was deepithelialised extraorally using a 15C scalpel blade in order to obtain a connective tissue graft from the underlying layer18.
The de-epithelialised graft was inserted and
positioned buccally and occlusally using horizontal mattress sutures with 5-0 non-resorbable suture (Figure 4)19.
Post-surgical medication included an antibiotic (1 g of amoxicillin twice daily for 7 days) and an antiinflammatory (25 mg of dexketoprofen three times daily for 5 days). The sutures were removed 10 days after the procedure.
* Phase III: three months after implant placement, the soft tissue condition was favourable (Figures 5 and 6). A digital impression was obtained using an intraoral scanner for the fabrication of a screwretained
polymethyl methacrylate (PMMA) provisional restoration. Regarding the definitive
implant crown, a cement-screw-retained
restoration was fabricated with a titanium nitride interface, adapting the design to the emergence profile already consolidated with the provisional prosthesis. The crown was produced by CAD-CAM in zirconia with full reduction and feldspathic ceramic veneering for zirconia (Figure 7).
1.3 Digital measurements of the augmented
vestibular soft tissue.
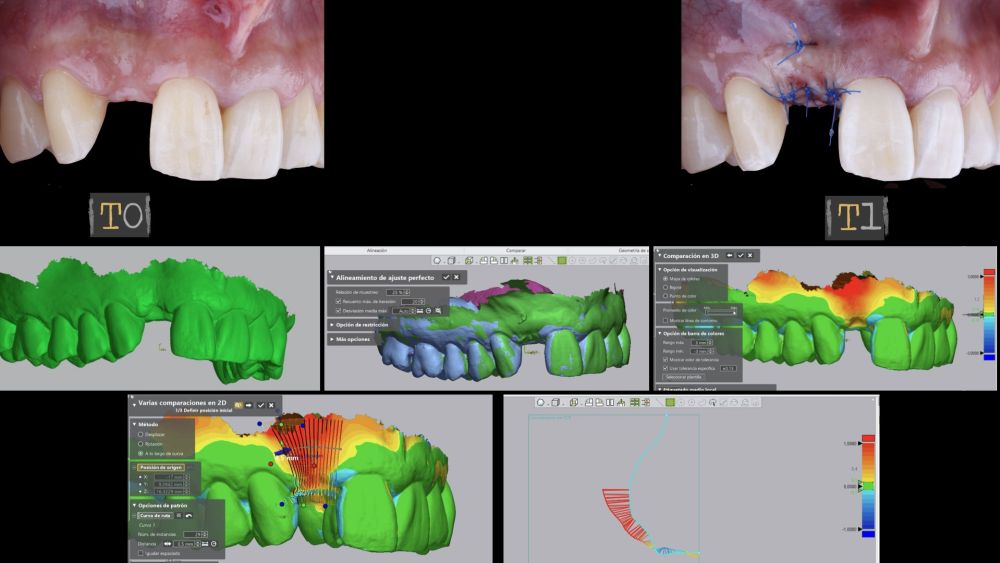
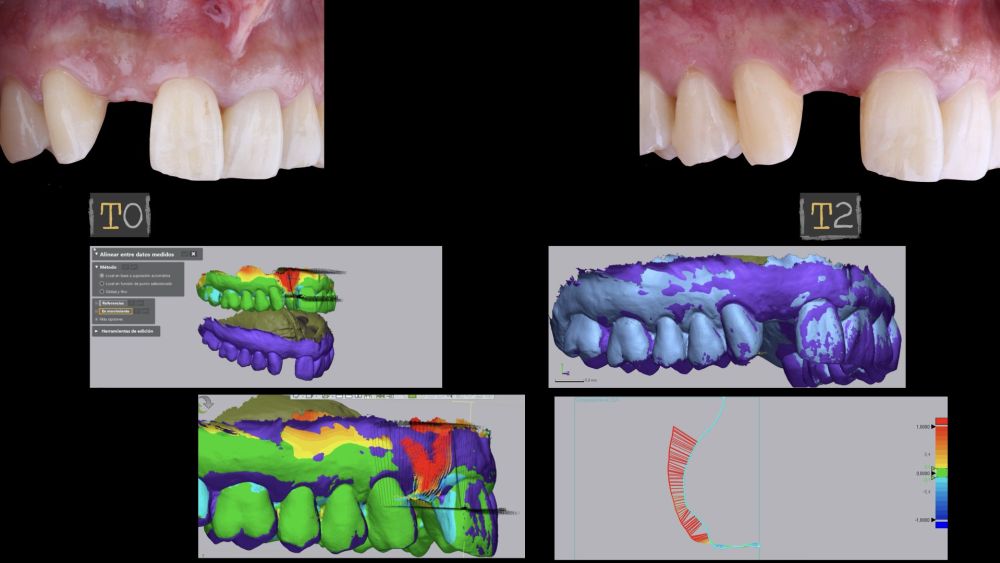
The site where the surgery was performed (implant 1.2), together with its complete arch, was scanned using an
intraoral optical scanner at different time points; three
weeks before the surgery (T0), immediately after the surgery (T1), and one and a half months post-surgery (T2). The generated digital models were exported and saved as STL files to be subsequently imported into image analysis software (Geomagic® Control X™; 3D
Systems, Rockhill, SC). An analysis of preoperative (T0) versus postoperative (T1 and T2) thickness changes was conducted. These longitudinal thickness changes were analysed on the vestibular aspect of the implantsupported crown using the “3D Compare” function, which
enabled the creation of a colour map following model superimposition to quantitatively assess the variations occurring in the intervention areas. The colour map ranges from +3 mm to -3 mm, with a tolerance of ± 0.15mm, and is interpreted as follows: green areas correspond
to perfect alignment of the models; red, orange, and yellow colours are interpreted as volume gain, while dark and light blue colours respectively represent volumetric loss (Figures
8 and 9). Subsequently, a rectangular region of interest was designed to study the intervention area, where linear changes of the peri-implant mucosa were evaluated (Figures 8 and 9). The horizontal extension of the region of interest encompassed both papillae (mesial and distal), covering the marginal contour of the implant crown up to the marginal surface of the adjacent teeth. To report the results of interest, points were identified on the horizontal plane previously designed on the vestibular aspect of the implant, starting from the mesial and extending 0.5 mm distally. Positive values indicated that the peri-implant soft tissues were located more buccally (> thickness), whereas negative values indicated that the peri-implant soft tissues were located more palatally (< thickness).
The final clinical outcome was satisfactory, fulfilling the patient’s aesthetic requirements. The soft tissues were morphologically and dimensionally stable, with no signs of
inflammation. However, changes in the peri-implant soft tissue (vestibular volumetric thickness) were demonstrated both qualitatively and quantitatively (Figures 8 and 9). In the immediate postoperative period (T1), the mean gain obtained when comparing T0 to T1 was 0.88 ± 0.15 mm, with a maximum increase of 1.1 mm. When comparing T0– T2, a mean gain of 0.73 ± 0.23 mm was observed. That is,
a volume contraction of 0.16 mm occurred from the time of graft placement (T1) until one and a half months later (T2).
The loss of a tooth in the aesthetic sector represents a challenge for the clinician, as it requires a multidisciplinary and comprehensive approach to restore function and aesthetics. To optimise aesthetic outcomes and reduce the dimensional bone changes that occur following tooth extraction, the use of bone substitutes has demonstrated advantages compared to alveolar healing without bone grafts20,21. Regarding the use of autologous platelet-rich fibrin in platelets and leukocytes, Pichotano et al. demonstrated that its application, together with a xenograft in bone regeneration, accelerates the bone healing process, resulting in an increase in new bone formation22.
Conversely, the use of connective tissue grafts is considered the technique of choice to compensate for the contraction of peri-implant soft tissues, thereby favouring pink aesthetics. Sharma et al. In their clinical study, gingival measurements were taken around the maxillary and mandibular lateral incisors23. These authors found that mean gingival thickness ranged between 0.56 and 1.02 mm. These mean values indicate or recommend increasing mucosal thickness over implants, as the patient’s own tissues are not sufficiently thick (<2 mm mucosal thickness)8.
In the present clinical case, a de-epithelialised connective tissue graft was placed on the buccal and occlusal aspects, resulting in greater mucosal thickness and increased height of the supracrestal tissue. The literature describes the advantages of peri-implant soft tissue augmentation, which is beneficial not only to minimise recession of the buccal mucosa but also to support peri-implant bone stability9,23–25. The study by Thoma et al. With a follow-up period of up to 3 years, they observed minimal changes in peri-implant soft tissue thickness at implant sites previously grafted with a xenogeneic membrane (-0.2 mm) compared to a subepithelial connective tissue graft (-0.1 mm)26. Furthermore, they found greater increases in mucosal thickness with the use of autologous connective tissue grafts compared to the xenogeneic substitute (on average 0.3 mm greater with autologous connective tissue grafts). However, the data obtained in our study regarding mucosal thickness cannot be compared with that of Thoma et al., as our study has a short follow-up period (approximately one and a half months) and only analyses the changes occurring between T0–T1 and T0–T2, without assessing the initial peri-implant mucosal tissue thickness26. In our study, it was observed that between T1 and T2 the connective tissue graft undergoes contraction during its healing process (an average of 0.16 mm).
Furthermore, guided implant surgery has been described in the literature as a promising technique that enhances accuracy both in pre-surgical planning and implant placement3. Additionally, tooth-supported surgical guides exhibit greater accuracy compared to bone-supported guides27. Similarly, the use of a tooth-supported guide without raising extensive flaps may be the optimal choice for both the clinician and the patient28. Moreover, virtual planning enables optimisation of implant placement in areas with complex anatomy and bone atrophy by allowing direct visualisation of the available bone volume29. Conversely, it provides the possibility of performing immediate loading procedures in a safe and predictable manner28.
Among the limitations associated with this technique are its higher cost compared to the conventional approach, potential fractures of the surgical guide during the intervention, and the requirement to be conducted under favourable anatomical conditions, as it necessitates the use of specialised instruments that may be limited to cases without restricted mouth opening. Moreover, the fabrication of an immediate provisional restoration may be compromised by minor discrepancies between the actual and planned implant positions, potentially resulting in slight misfits3,29–32. An additional disadvantage concerning the various phases of the presented surgical protocol is the increased number of surgical procedures performed
The presented case exemplifies a multidisciplinary approach to the loss of a tooth in the aesthetic sector. It is important to emphasise that meticulous management of hard and soft tissues, as well as planning via guided surgery, enhances precision concerning the ideal position from a prosthodontic standpoint, thereby influencing the long-term stability of hard and soft tissues. The present volumetric analysis suggests that following the execution of a connective tissue graft, there is an initial gain which diminishes after one and a half months.
Vercruyssen M, Laleman I, Jacobs R, et al. Computer-supported implant planning and guided surgery: a narrative review. Clin Oral Implants Res. 2015;26(S11):69- 76.
Tatakis DN, Chien HH, Parashis AO. Guided implant surgery risks and their prevention. Periodontol 2000. 2019;81(1):194-208.
Pimkhaokham A, Jiaranuchart S, Kaboosaya B, et al. Can computer- assisted implant surgery improve clinical outcomes and reduce the frequency and intensity of complications in implant dentistry? A critical review. Periodontol 2000. 2022;90(1):197-223.
Apostolakis D, Brown JE. The anterior loop of the inferior alveolar nerve: prevalence, measurement of its length and a recommendation for interforaminal implant installation based on cone beam CT imaging. Clin Oral Implants Res. 2012;23(9):1022-1030.
Romandini M, Ruales-Carrera E, Sadilina S, et al. Minimal invasiveness at dental implant placement: A systematic review with meta-analyses on flapless fully guided surgery. Periodontol 2000. 2023;91(1):89-112.
Chackartchi T, Romanos GE, Parkanyi L, et al. Reducing errors in guided implant surgery to optimize treatment outcomes. Periodontol 2000. 2022;88(1):64-72.
Ávila G, González O, Couso E, et al. The peri-implant phenotype. J Periodontol. 2020;91(3):283-288.
Monje A, González O, Ávila G. Impact of peri-implant soft tissue characteristics on health and esthetics. J Esthet Restor Dent. 2023;35(1):183-196.
Thoma DS, Gasser TJW, Hämmerle CHF, et al. Soft tissue augmentation with a volume-stable collagen matrix or an autogenous connective tissue graft at implant sites: Five-year results of a randomized controlled trial post implant loading. J Periodontol. 2023;94(2):230- 243.
Thoma DS, Strauss FJ, Mancini L, et al. Minimal invasiveness in soft tissue augmentation at dental implants: A systematic review and meta-analysis of patient-reported outcome measures. Periodontol 2000. 2023;91(1):182-198.
Tavelli L, Barootchi S, Ávila G, et al. Peri-implant soft tissue phenotype modification and its impact on peri- implant health: A systematic review and network meta-analysis. J Periodontol. 2021;92(1):21-44.
Ávila G, Couso E, Pirc M, et al. Outcome measures and methods of assessment of soft tissue augmentation interventions in the context of dental implant therapy: A systematic review of clinical studies published in the last 10 years. J Clin Periodontol. 2023;50(S25):83-95.
Wismeijer D, Joda T, Flügge T, et al. Group 5 ITI Consensus Report: Digital technologies. Clin Oral Implants Res. 2018;29(S16):436-442.
Fan S, Sáenz-Ravello G, Al-Nawas B, et al. The feasibility of ultrasonography for the measurement of periodontal and peri-implant phenotype: A systematic review and meta-analysis. Clin Implant Dent Relat Res. 2023;25(5):892-909.
Pirc M, Harbeck O, Sapata VM, et al. Contour changes of peri-implant tissues are minimal and similar for a one- and a two-piece implant system over 12 years. Clin Oral Investig. 2021;25(2):719-727.
Strauss FJ, Gil A, Smirani R, et al. The use of digital technologies in peri-implant soft tissue augmentation – A narrative review on planning, measurements, monitoring and aesthetics. Clin Oral Implants Res. 2024 (2). doi:10.1111/ clr.14238.
Fernandes D, Marques T, Borges T, et al. Volumetric analysis on the use of customized healing abutments with or without connective tissue graft at flapless maxillary immediate implant placement: A randomized clinical trial. Clin Oral Implants Res. 2023;34(9):934- 946.
Zucchelli G, Mele M, Stefanini M, et al. Patient morbidity and root coverage outcome after subepithelial connective tissue and de-epithelialized grafts: a comparative randomized-controlled clinical trial. J Clin Periodontol. 2010;37(8):728-738.
González D, Cabello G, Olmos G, et al. The saddle connective tissue graft: a periodontal plastic surgery technique to obtain soft tissue coronal gain on immediate implants. A case report. Int J Esthet Dent. 2015;10(3):444-455.
Araújo MG, da Silva JCC, de Mendonça AF, et al. Ridge alterations following grafting of fresh extraction sockets in man. A randomized clinical trial. Clin Oral Implants Res. 2015;26(4):407-412.
Sanz M, Lindhe J, Alcaraz J, Sanz- Sanchez I, et al. The effect of placing a bone replacement graft in the gap at immediately placed implants: a randomized clinical trial. Clin Oral Implants Res. 2017;28(8):902-910.
Pichotano EC, de Molon RS, Freitas de Paula LG, et al. Early Placement of Dental Implants in Maxillary Sinus Grafted With Leukocyte and Platelet-Rich Fibrin and Deproteinized Bovine Bone Mineral. J Oral Implantol. 2018;44(3):199-206.
Sharma S, Thakur SL, Joshi SK, et al. Measurement of gingival thickness using digital vernier caliper and ultrasonographic method: a comparative study. J Investig Clin Dent. 2014;5(2):138-143.
Lee CT, Tao CY, Stoupel J. The Effect of Subepithelial Connective Tissue Graft Placement on Esthetic Outcomes After Immediate Implant Placement: Systematic Review. J
Frizzera F, de Freitas RM, Muñoz- Chávez OF, et al. Impact of Soft Tissue Grafts to Reduce Peri-implant Alterations After Immediate Implant Placement and Provisionalization in Compromised Sockets. Int J Periodontics Restorative Dent. 2019;39(3):381-389.
Atieh MA, Alsabeeha NHM. Soft tissue changes after connective tissue grafts around immediately placed and restored dental implants in the esthetic zone: A systematic review and meta-analysis. J Esthet Restor Dent Off Publ Am Acad Esthet Dent Al. 2020;32(3):280-290.
Thoma DS, Gasser TJW, Jung RE, et al. Randomized controlled clinical trial comparing implant sites augmented with a volume-stable collagen matrix or an autogenous connective tissue graft: 3-year data after insertion of reconstructions. J Clin Periodontol. 2020;47(5):630-639.
Raico Gallardo YN, da Silva-Olivio IRT, Mukai E, et al. Accuracy comparison of guided surgery for dental implants according to the tissue of support: a systematic review and meta-analysis. Clin Oral Implants Res. 2017;28(5):602-612.
Gargallo J, Barootchi S, Salomó O, et al. Advantages and disadvantages of implant navigation surgery. A systematic review. Ann Anat – Anat Anz. 2019;225:1-10.
D’haese J, Ackhurst J, Wismeijer D, et al. Current state of the art of computer- guided implant surgery. Periodontol 2000. 2017;73(1):121-133.
Smitkarn P, Subbalekha K, Mattheos N, et al. The accuracy of single-tooth implants placed using fully digital-guided surgery and freehand implant surgery. J Clin Periodontol. 2019;46(9):949-957.
Tattan M, Chambrone L, González- Martín O, et al. Static computer-aided, partially guided, and free-handed implant placement: A systematic review and meta-analysis of randomized controlled trials. Clin Oral Implants Res. 2020;31(10):889-916.
Quispe N, Flores J, Pardal B, et al. Factors Influencing the Accuracy of Guided Surgery: An In Vitro Trial. Int J Oral Maxillofac Implants. 2023;38(1):120-129.

Quispe López, Norberto
Associate Lecturer, Department of Surgery, Stomatology Area, University of Salamanca (USAL).
Dahdouh, Manar
5th-year Dentistry student, University of Salamanca.
Ledesma Sánchez, Lucía
5th-year Dentistry student, University of Salamanca.
Rodríguez Muñoz, Pablo
4th-year Dentistry student, University of Salamanca.