Clinical case
Published in spanish Científica Dental Vol. 19. Nº 3. 2022
Integral surgical and orthodontic treatment of an autotransplanted maxillary canine: case report
Introduction: The main treatment of impacted canines is orthodontics. In case of failure, extraction of the canine and the subsequent placement of a dental implant is given as an alternative. Autotransplantation is considered a treatment option as long as the full extraction of the canine is viable, because it provides many advantages as the ability of mobilization with orthodontics
Case report: Description of a clinical case in which an autotransplantation of an included canine was carried out after traction failed in a young patient. After regenerative surgery was realized in its surroundings the patient underwent orthodontic and restorative treatment. 18 months of follow–up later the patient remains asymptomatic, with no mobility or resorption signs and with a healthy periodontal state in said canine.
Conclusion: Autotransplantation can be a suitable alternative when orthodontic traction has failed, as long as it is viable, especially in young patients when implants are not recommended.
Included canines are considered those that, at their normal eruption age (13.9 years in women and 14.6 years in men), remain retained in the jaw surrounded by the pericoronary sac and with their bone tissue intact1. The prevalence of impacted teeth varies between 5.6 and 18.8%, being the maxillary canines up to 2% of the total impacted teeth2.
The treatment of choice against impacted canines is orthodontic traction to guide them to their ideal position, which is not always viable due to factors such as the location of the canine, age or the refusal of the patient to undergo orthodontic treatment. Faced with this impossibility of conservative traction treatment, two treatment philosophies are presented: the expectant attitude with follow-up periods, leaving the impacted canine while it does not cause any pathology, or the extraction of the same2.
Exodontia is usually associated with the insertion of a dental implant and its rehabilitation with an implant-supported prosthesis. But an alternative to inserting alloplastic grafts is autotransplantation, an ideal replacement of the tooth in the dental arch2,3. Autotransplantation is defined as the process of moving an impacted or erupted tooth from one site to another in the same individual, either to a natural alveolus or surgically created, usually with implant drills3,4. This technique is considered an alternative with an adequate success rate to rehabilitate function and aesthetics, especially in young patients5.
The aim of this article is to describe a clinical case in which an autotransplantation of an impacted canine after failure of the orthodontic traction was performed in a young patient who was subsequently subjected to orthodontic and restorative treatment.
Description of the case
A 13-year-old female patient, with no previous medical history, attends the Master of Dentofacial Orthopaedics at the Universidad Rey Juan Carlos (URJC) where she is diagnosed with an impacted 2.3. For this, she is sent to the Master of Oral Surgery and Implantology of the same University. A bone window is made through which the crown of the canine is exposed, to finally adhere an orthodontic button and perform traction.
After 17 months since said surgery, it is observed that the canine has not moved and it is decided to try the autotransplantation of the same.
Diagnostics
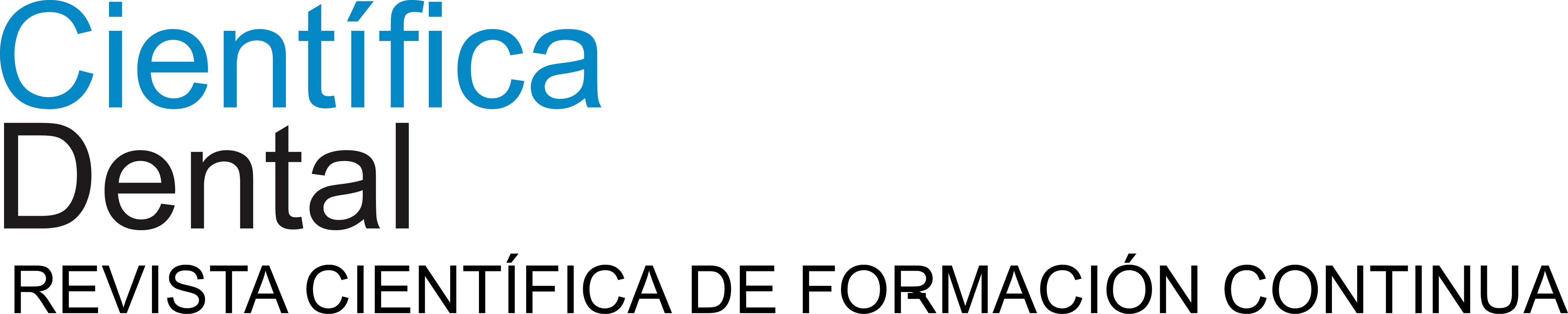
A conical beam computed tomography (CBCT) scan is performed to evaluate the exact position of the impacted canine which is located in mixed position, with the root completely formed in Nolla6 stage 10 and Moorrees stage 67, in contact with the cortical of the sinus and the crown with the cusp breaking the vestibular cortical. Around the crown a radiolucency is observed that corresponds to the pericoronary sac.
Regarding the adjacent teeth, no resorption of the roots was observed in the radiological tests and the clinical examination showed positive vitality and no discomfort on percussion.
Planning
Measurements were made with the CBCT to determine the exact dimensions of the canine and the receiving area to ensure that the space was correct and was not necessary to modify it with orthodontics. In addition, anatomical relationships with adjacent structures were evaluated to avoid possible complications during surgery (Figure 1).
Surgical treatment
Local supraperiosteal anaesthesia (Articaina 4%, 1:100000 IU) was administered at the bottom of the vestibule from the lateral incisor of the first quadrant (1.2) to the first molar of the second quadrant (2.6).
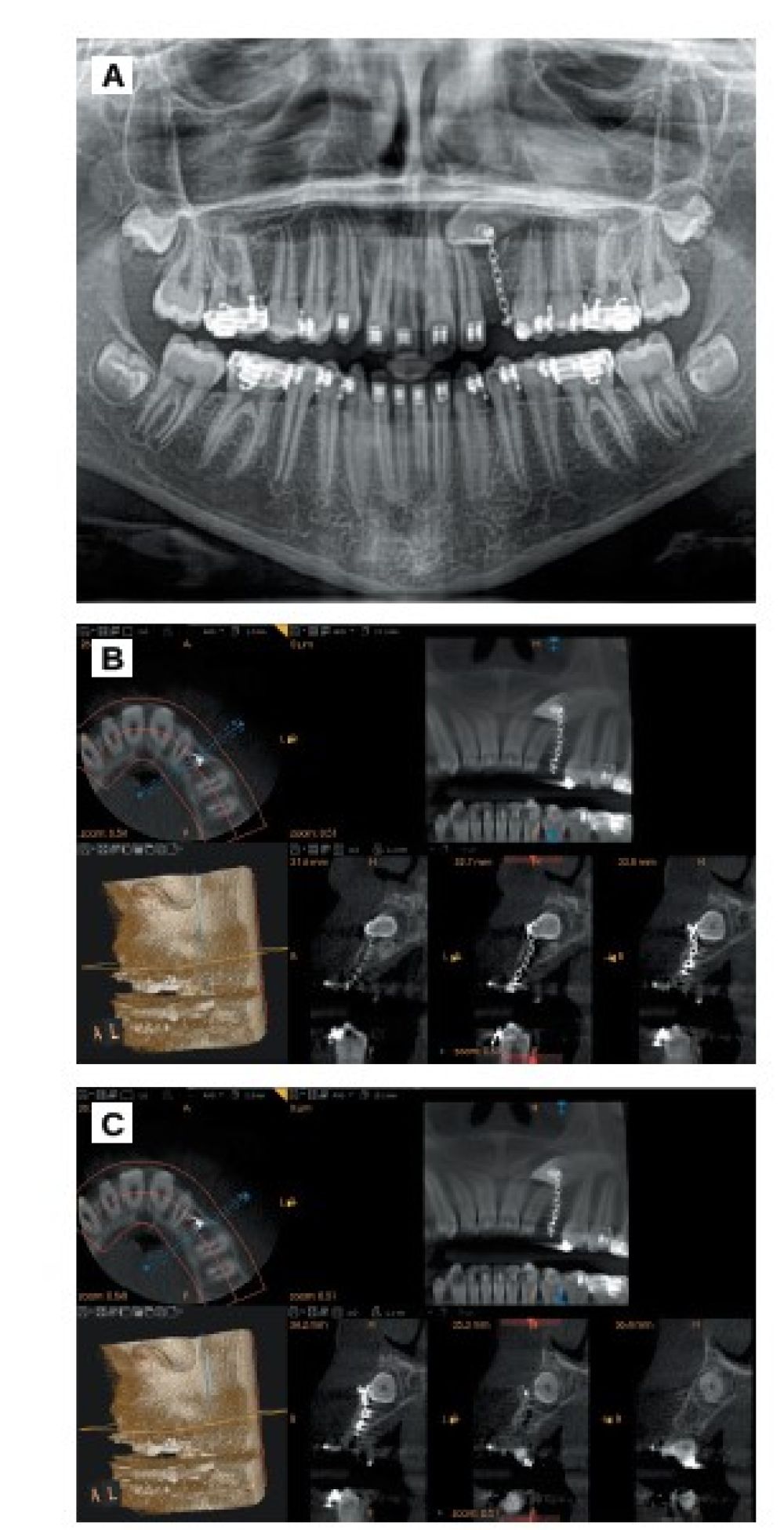
Both the anterior palatine nerve and the nasopalatine nerve were anaesthetized.
Intrasulcular incisions and a crestal incision were made in the edentulous space of the left upper canine (2.3). A vestibular flap was lifted at total thickness from the first left upper molar (2.6) to the contralateral lateral incisor (Figure 2). Using a round osteotomy drill number 8 from a hand piece, a vestibular bone window was made until the whole canine crown was exposed (Figure 2). The tooth was then loosened using two elevators, without exceeding the amelocementary limit to avoid damaging the periodontal ligament fibres (Figure 2).
The osteotomy was performed in the crestal region in order to make a surgical alveolus (Figure 2) with an anatomy similar to the future canine autotransplantation using surgical implant drills from the same business (Biomet 3i, Barcelona, Spain). A tooth exodontia was performed (Figure 2) and moved to the surgical alveolus (Figure 2). Guided bone regeneration was performed in the vestibular and palatal region of the same, both to surround the tooth in a favourable bone frame and to regenerate the vestibular defect that remained after the extraction of the canine.
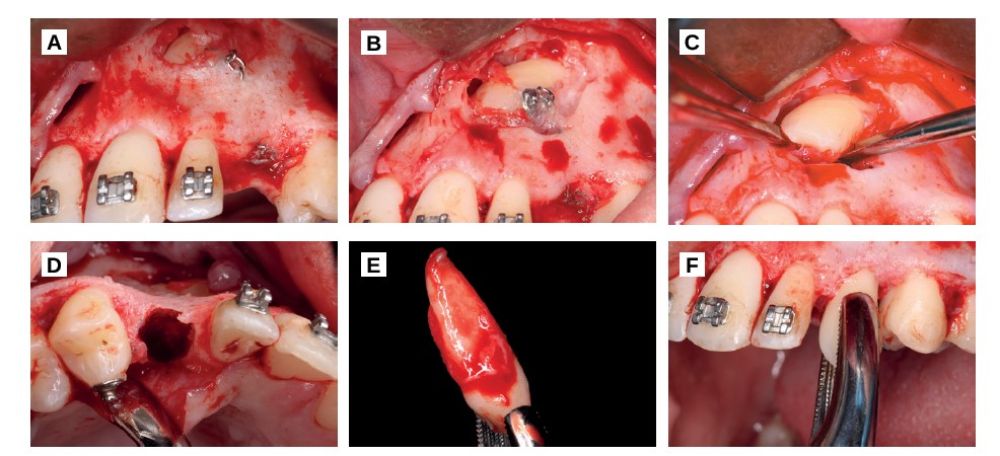
For palatal regeneration, local supraperiosteal infiltrative anaesthesia was placed in the bottom of the lower molars of the 4th quadrant and an intrasulcular incision was made in the first and second right lower molar (4.6 and 4.7) that was continued with a linear incision through the mandibular ramus. The total thickness of the vestibular flap was detached and autologous particulate bone of the mandibular ramus was obtained with a bone scraper (Figure 3). Once enough autologous bone was obtained, the retromolar gap was stitched with 5/0 monofilament suture with simple stitches.
In the palatine a titanium mesh was placed fixed with two osteosynthesis screws (Stryker, Michigan, USA).
The created space was filled with particulate autologous bone mesh in order to regenerate the area of the tooth that was outside the bone (Figure 3) and the vestibular was regenerated with biomaterial (Apatos, Osteógenos, Madrid, Spain), since it was a self-contained cavity (Figure 3).
Finally, the flap was sutured with simple stitches repositioning the papillae, with a monofilament suture 5/0. The occlusion was reduced until it did not make contact with any other tooth and the canine was ferulized with the orthodontic arch itself (Figures 3 and 3) for 2 weeks.
Postoperative antibiotic (amoxicillin + clavulanic acid 875/125), anti-inflammatory (Dexketoprofen 25mg) and analgesics (paracetamol 1g) were prescribed for 7 days.
Endodontic treatment
After 2 weeks of the surgery, periapical X-rays were taken and a root canal of the canine was performed under absolute isolation (Figure 3).
The ferulization was removed and it was verified that the tooth had no mobility or percussion sensitivity.
Orthodontic treatment
After two weeks of the root canal, orthodontic movements started in order to place the canine in a correct position in the arch. For this, fixed brackets and arches were used, first of 0.16 nickel titanium (NiTi) and later of 16×4 NiTi x16.
Completion of the case and aesthetic treatment
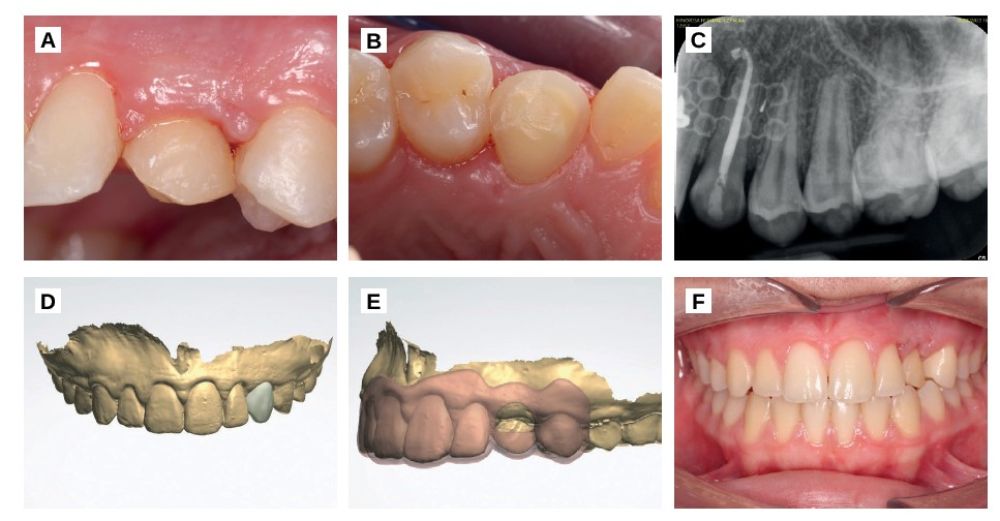
After a follow-up of 12 months, the brackets were removed. The patient was asymptomatic and the canine did not feel mobility or any pathology signs to clinical and radiographic examination (Figures 4A, 4B, 4C). Finally a crown elongation was performed to level the gingival margin to the contralateral canine. A guided surgery splint was planned, based on a previous digital waxing, which marked the position of both the new gingival margin and the bone level (Figures 4D, 4E, 4F).
Once the gum is stabilized, the aesthetic result will be improved with a composite veneer.
The prevalence of inclusion of the upper canines varies according to the literature. Zufia et al.2 describe a 2% of the general population. Most canine inclusions occur in the maxilla, with a prevalence of 1 – 3% compared to 0.07 – 3% in the jaw8.
The aetiology of inclusion is considered multifactorial, two thirds of the upper canines retention take place in the palate, of which, 85% have space to erupt but are impacted due to a very complex eruption trajectory or genetic factors. The remaining third are retained in the vestibular bone, in most cases due to lack of space due to maxillary compression1-9.
The first treatment option in any scenario will always be orthodontic traction, either with open or closed window. It is a treatment that offers good results but is not always viable, either because of a high position of the canine or simply because of the refusal of the patient to undergo a long and expensive orthodontic treatment2. Davarpanah et al. mention success rates of 100% in patients up to 20 years of age, while in adults (between 20 and 47 years of age) success rates of 69.5% of the described cases8.
When traction is not feasible, different treatment options are described, including autotransplantation of the included canine, extraction and placement of an implant3, or even some articles break with the principles of osseointegration and describe the placement of an implant through the included canine without performing the extraction10.
To plan a case of these characteristics, it must be taken into account that autotransplantation, unlike implants, adapts to the eruption, it can be moved with orthodontics, stimulates bone regeneration, maintains proprioception and preserves the gingival architecture of the ligament3-11. In addition, it delays the placement of implants, constituting an alternative if the autotransplantation does not work12.
One of the keys to the success of autotransplantation is a healthy periodontal state, therefore, extraction should be as atraumatic as possible. Extraoral tooth time is also a key factor. Ji – Hyun et al. performed a series of 19 cases where the extraoral time was between 3 and 16 minutes, with a success of 84% of cases; to reduce the risk of complications the tooth should not exceed 18 minutes out of mouth13. The included canines, being teeth that have never had occlusion, have a periodontal ligament that is poorer in fibres, which is why some authors propose the application of orthodontic forces prior to autotransplantation surgery4. Phutinart et al. observed changes in the periodontal ligament after one, two, three and four weeks of orthodontics and found that the ligament size reached its maximum level after applying forces for one month14. That is why, in included canines, it is advisable to try orthodontic traction prior to surgery to increase the fibres of the periodontal ligament, since it is demonstrated that an early application of orthodontic forces increases the autotransplantation success rate15. In addition, it can be favourable, when placing the canine in a better position to facilitate extraction and achieve occlusal space before autotransplantation4. Autotransplantation success rates are described at 98%4, 90% for included canines16 and 93% when they have been subsequently treated with orthodontics15z.
According to the studies consulted, orthodontic movements can begin to be performed between four and eight weeks after surgery, after the endodontic treatment has been completed and the ferulization removed15. Keep in mind that if ferulization exceeds six weeks, the ankylosis risk increases, then it will be much more difficult to move it with orthodontics7. Another possible complication is the resorption of the root, which occurs if during surgery the periodontal ligament of the tooth is damaged, since the formation of bone over dentin is stimulated. Resorption rates may increase if orthodontic forces are very large. Lacerda-Santos et al. indicate that resorption associated with orthodontic treatment ranges between 6 and 64%. Therefore, in autotransplanted teeth the forces applied must be minimal17.
Autotransplants are also an option that allows combining different regenerative techniques. In the case described, it was decided to regenerate the palatal area with autologous scratched bone of the ramus since it is an area where a particulate is obtained with many morphogenetic proteins (BMPs), therefore, it increases the osteogenic capacity of the graft making it suitable to regenerate defects outside the bone18.
The autotransplantation of included canines is, therefore, a technique that provides advantages such as greater proprioception, the possibility of moving them with orthodontics or immediacy in young patients where the placement of implants is not feasible. However, it is a sensitive technique that depends on the experience of the operator, the conservation of the periodontal ligament or the position of the canine among other factors. These disadvantages, coupled to the lack of scientific evidence from the articles in which the technique is described, make it difficult to evaluate the effectiveness of the same.
Autotransplantation of included maxillary canines is an alternative to implant placement when orthodontic traction is not viable. It should be emphasized the importance of good planning, the possibility of the full extraction of the canine according to its relationship with adjacent anatomical structures and a good conservation of the periodontal ligament. It can also be combined with regeneration and orthodontic procedures whenever necessary.
More studies with more scientific evidence are needed to objectively evaluate the success rates of this technique.
Dr. Alejandro Félix: Master Degree Student of Microscopic Endodontics and Apical Surgery of Universidad Rey Juan Carlos.
Dr. Marcela Salamanca: Professor of Master of Microscopic Endodontics and Apical Surgery of Universidad Rey Juan Carlos.
Dr. Sofía Sánchez: Master Degree Student of Orthodontics and Dentofacial Orthopaedics of Universidad Rey Juan Carlos.
Dr. Pablo Castillo: Master Degree Student of Orthodontics and Dentofacial Orthopaedics of Universidad Rey Juan Carlos.
Dr. Carolina Nieto: Professor of Master of Orthodontics and Dentofacial Orthopaedics of Universidad Rey Juan Carlos.
Grisar K, Chaabouni D, Romero LPG, Vandendriessche T, Politis C, Jacobs R. Autogenous transalveolar transplantation of maxillary canines: a systematic review and meta-analysis. Eur. J. Orthod. 2018; 40 (6): 608.
Zufía J, Abella F, Gómez-Meda R, Blanco H, Roig M. Autotransplantation of impacted maxillary canines into surgically modified sockets and orthodontic treatment: a 4-year follow-up case report. Int. J. Esthet. DENT. 2020; 15 (2): 96-210.
Izadikhah I, Cao D, Zhao Z, Yan B. Different Management Approaches in Impacted Maxillary Canines: An Overview on Current Trends and Literature. J. Contemp. Dent. 2020 01; 21 (3): 326-336.
Hariri R, Alzoubi EEM. Autotransplantation in combination with orthodontic treatment.
J. Orthod. Sci. 2019; 8 (1): 11.
Kafourou V, Tong HJ, Day P, Houghton N, Spencer RJ, Duggal M. Outcomes and prognostic factors that influence the success of tooth autotransplantation in children and adolescents. Dent. Traumatol. 2017; 33 (5): 393-399.
Tomás LF, Mónico LSM, Tomás I, Varela-Patiño P, Martin-Biedma B. The accuracy of estimating chronological age from Demirjian and Nolla methods in a Portuguese and Spanish sample. BMC oral health 2014; 14 (1): 160.
Sicilia-Pasos J, Kewalramani N, Peña- Cardelles JF, Salgado-Peralvo AO, Madrigal-Martínez-Pereda C, López- CarpinteroÁ. Autotransplantation of teeth with incomplete root formation: systematic review and meta-analysis. Clin. Oral. Investig. 2022; 26 (5): 3795-3805.
Davarpanah M, Szmukler-Moncler S, Rajzbaum P, Davarpanah K, Capelle-Ouadah N, Demurashvili G. Unconventional implant placement. V: Implant placement through impacted teeth; results from 10 cases with an 8- to 1-year follow-up. Int. Orthod. 2015; 13 (2): 164-180.
Bedoya MM, Park JH. A review of the diagnosis and management of impacted maxillary canines. J. Am. Dent. Assoc. 2009; 140 (12): 1485-93.
GB F. Immediate Implant Post-Extraction of Impacted Maxillary Canine: Systematic Review. Open Access J. Dent. Sci. 2017; 2 (2).
Lucas-Taulé E, Llaquet M, Muñoz- Peñalver J, Somoza J, Satorres-Nieto M, Hernández-Alfaro F. Fully Guided Tooth Autotransplantation Using a Multidrilling Axis Surgical Stent: Proof of Concept. J. Endod. 2020; 46 (10): 1515-1521.
Tsukiboshi M, Yamauchi N, Tsukiboshi Y. Long‐term outcomes of autotransplantation of teeth: A case series. Dent. Traumatol. 2019; 35 (6): 358-367.
Bae, Ji-Hyun, Choi, Yong-Hoon, Cho, Byeong-Hoon, Kim, Young-Kyun, Kim, Su-Gwan. Autotransplantation of Teeth with Complete Root Formation: A Case Series. J. Endod. 2010; 36 (8): 1422-1426.
Phutinart S, Krisanaprakornkit S, Makeudom A, Suzuki B, Suzuki EY. Periodontal ligament proliferation and expressions of bone biomolecules upon orthodontic preloading: Clinical implications for tooth autotransplantation. Korean J. Orthod. 2012 2020; 50 (3):188-196.
Kokai S, Kanno Z, Koike S, et al. Retrospective study of 100 autotransplanted teeth with complete root formation and subsequent orthodontic treatment. Am. J. Orthod. Dentofacial. Orthop. 2015; 148 (6): 982-989.
Grisar K, Denoiseux B, Martin C, et al. Treatment for critically impacted maxillary canines: Clinical versus scientific evidence – A systematic review. J. Stomatol. Oral Maxillofac. Surg. 2021 17.
Lacerda-Santos R, Canutto RF, Araújo, et al. Effect of Orthodontic Treatment on Tooth Autotransplantation: Systematic Review of Controlled Clinical Trials. Eur. J. Dent. 2020; 14 (03): 467.
Lacerda-Santos R, Canutto RF, Araújo, et al. Effect of Orthodontic Treatment on Tooth Autotransplantation: Systematic Review of Controlled Clinical Trials. Eur. J. Dent. 2020; 14 (03): 467.

Galán Valero, Elisa
Master Degree Student of Oral Surgery and Implantology at the Universidad Rey Juan Carlos.
Fontán García, Natalia
Master Degree Student of Oral Surgery and Implantology at the Universidad Rey Juan Carlos.
Asensio Acevedo, Ramón
Master Degree Student of Oral Surgery and Implantology at the Universidad Rey Juan Carlos.
Ortega Concepción, Daniel
Master Degree Professor of Oral Surgery and Implantology at the Universidad Rey Juan Carlos.
Flores Gallardo, Arturo
Master Degree Professor of Oral Surgery and Implantology at the Universidad Rey Juan Carlos.
Peña Cardelles, Juan Francisco
Surgery Master Degree Professor of Oral and Implantology at the Universidad Rey Juan Carlos.
Gómez de Diego, Rafael
Master’s Degree Director of Oral Surgery and Implantology at the Universidad Rey Juan Carlos.