Clinical case
Published in spanish Científica Dental Vol. 20. Nº 1. 2023
Maxillary reconstruction with a subperiosteal implant in a case of severe atrophy. From planning to rehabilitation following a fully digital protocol. About a clinical case and bibliographic review
Introduction: Customized subperiosteal titanium implants, designed from planning and fabrication software, constitute an alternative in the rehabilitation of severe maxillary atrophy, avoiding more complex bone and soft reconstruction surgeries and reducing healing times. The aim of this article is to present the rehabilitation in a clinical case with severe atrophy in the upper jaw, using a structure with subperiosteal implants, by means of a digital protocol.
Clinical Case: A subperiosteal sintered titanium structure was fabricated with six transepithelial connections that were rehabilitated with an immediate implant supported fixed prosthesis made of PMMA. Two months later, a sintered chromium-cobalt framework with machined bases covered with acrylic resin teeth was fabricated as the final restoration. At one year follow-up, the case remains stable.
Conclusions: Nowadays, rehabilitation with subperiosteal implants is an alternative tool in cases of complex surgeries with large atrophies with the possibility of immediate loading.
The use of endoosseous dental implants to replace the absence of teeth has shown a great predictability over the years, being today one of the main techniques for dental rehabilitation1. However, bone in quantity and quality is necessary for its placement. In cases of severe bone resorption, more advanced surgeries are needed for bone regeneration, in which there may be more complications, morbidity and longer treatment time2.
Subperiosteal implants (SI) were developed in Sweden in the early 1940´s. The SI consisted of a custom-made implant, inserted under the periosteum and fixed with screws and the mucous tissue that covered it3,4. They were manufactured in chromium-cobalt or titanium alloys and were rehabilitated by transmucous pillars that emerged in the oral cavity5. Although they were used for years in cases of maxilla atrophies, they were replaced by endoosseous implants designed by Branemark6. This was due to its complex manufacturing. It was necessary to take an impression of the residual bone ridge, which was sent to the laboratory for the structure design, with the consequent imbalances since they were not very stable models. In this way, its placement in the patient was very difficult, and several complications could appear7,8. However, advances in the planning and manufacturing field with various materials have allowed these structures to be made digitally with an excellent predictability and fit, thus avoiding more complex surgeries9.
The objective of this work is to present implant-supported rehabilitation in a clinical case with severe atrophy in the upper maxilla, using a structure with subperiosteal implants, through a digital protocol, and the evolution one year after its placement.
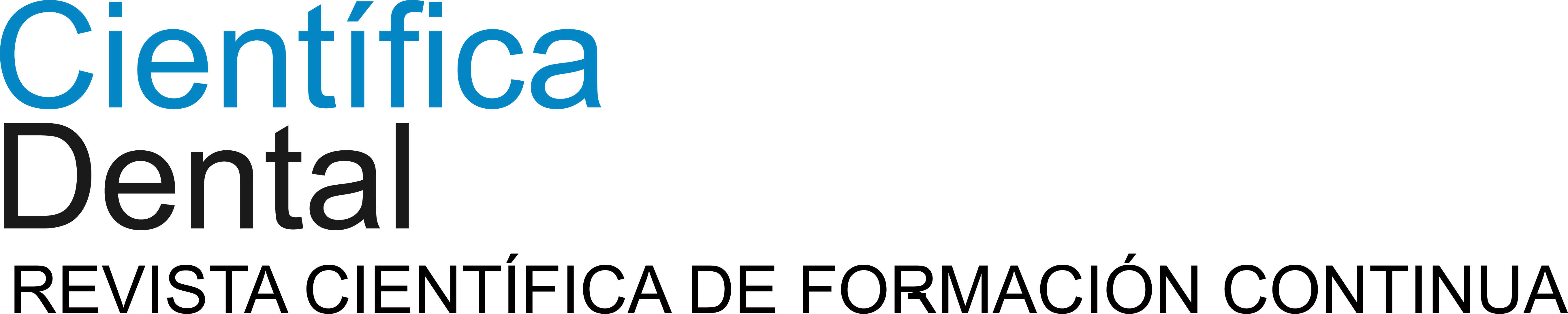
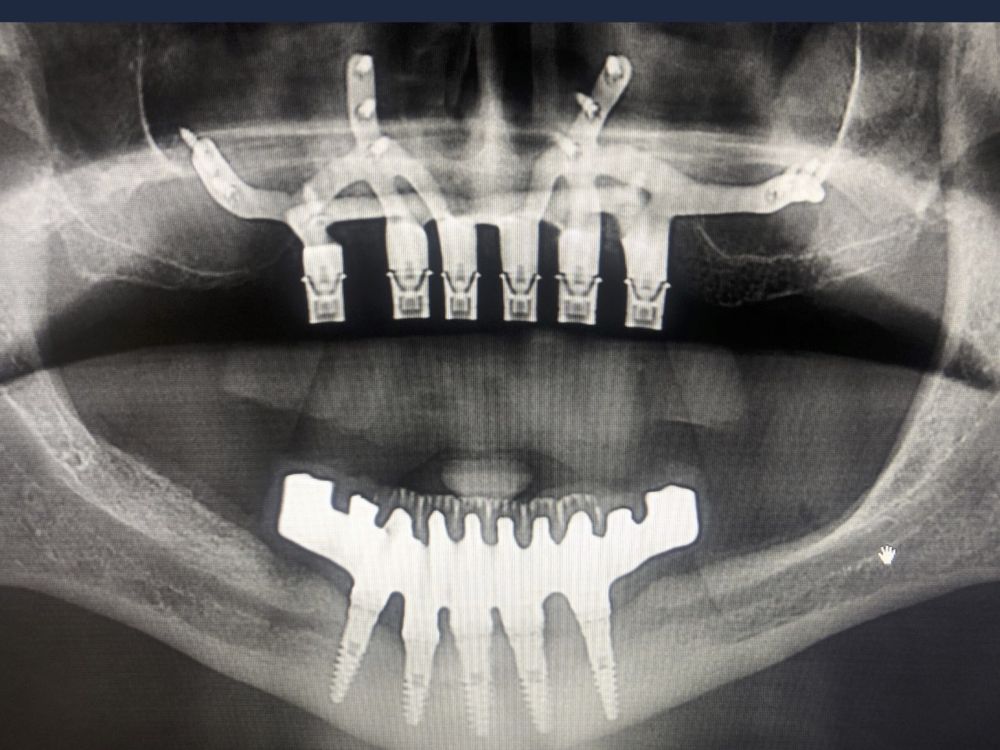
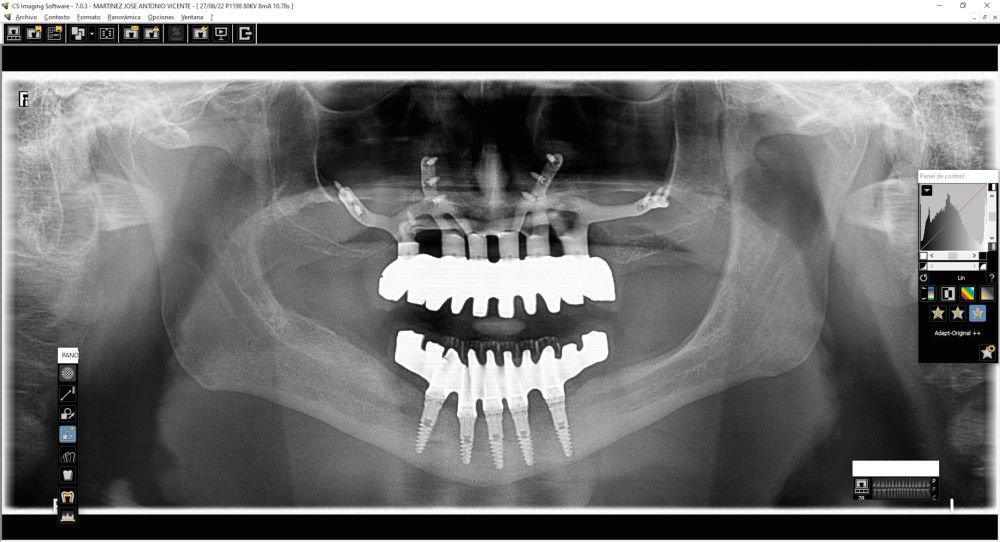
We present the clinical case of a 65-year-old patient with an implant-supported dentoalveolar rehabilitation on implants in the upper arch, placed in 2010, on which he referred pain, mobility and suppuration. After an orthopantomography, we observed a severe generalised perimplantitis in the upper arch, affecting all implants (Figure 1). It was explained to the patient that it was not possible to perform a bone regeneration of the lost tissues.
Under local anaesthesia, we disassembled the dentoalveolar hybrid prosthesis. It was only fixed by two implants that showed lower mobility. Periodontal curettage was performed in all areas adjacent to the lost implants and preprosthetic surgery to favour the closure of tissues with nonresorbable suture. A provisional complete prosthesis was placed during tissue healing time. Two months later, tissue healing was complete and no clinical signs of inflammation or pain were observed (Figure 2).
Given the degree of severe bone resorption after perimplantitis, the manufacture of an SI was planned as an alternative to the reconstruction of the upper maxilla with bone grafts, bilateral sinus lifts and subsequent placement of endosseal implants or surgery with zygomatic implants. With this type of reconstructions, it is also possible to perform an immediate load on the structure at the same time of the surgery.
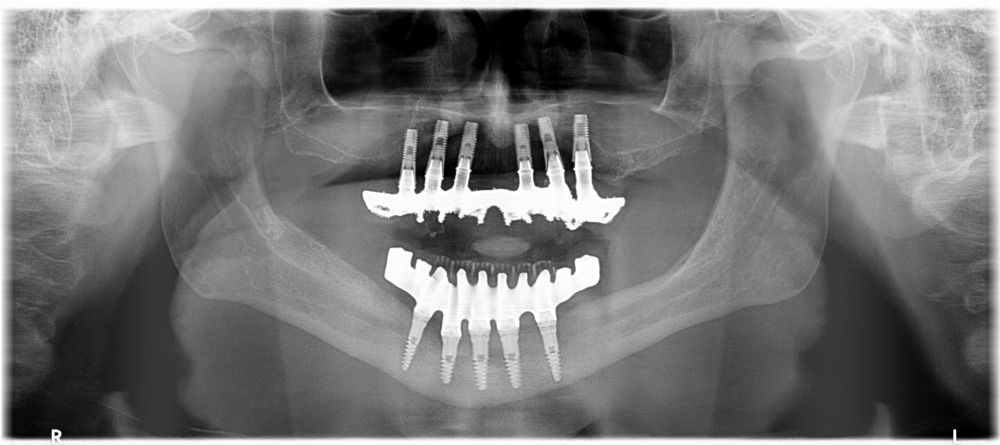
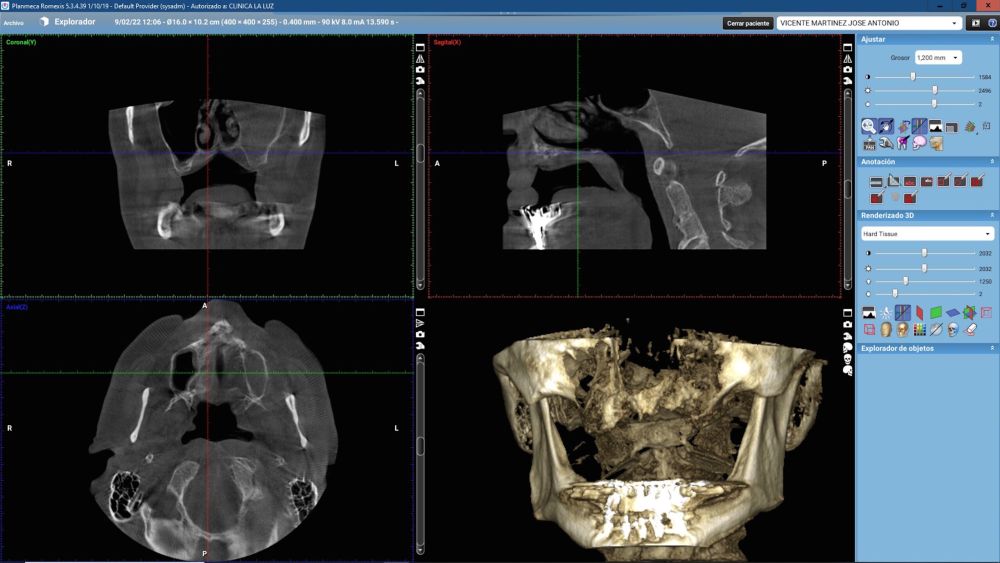
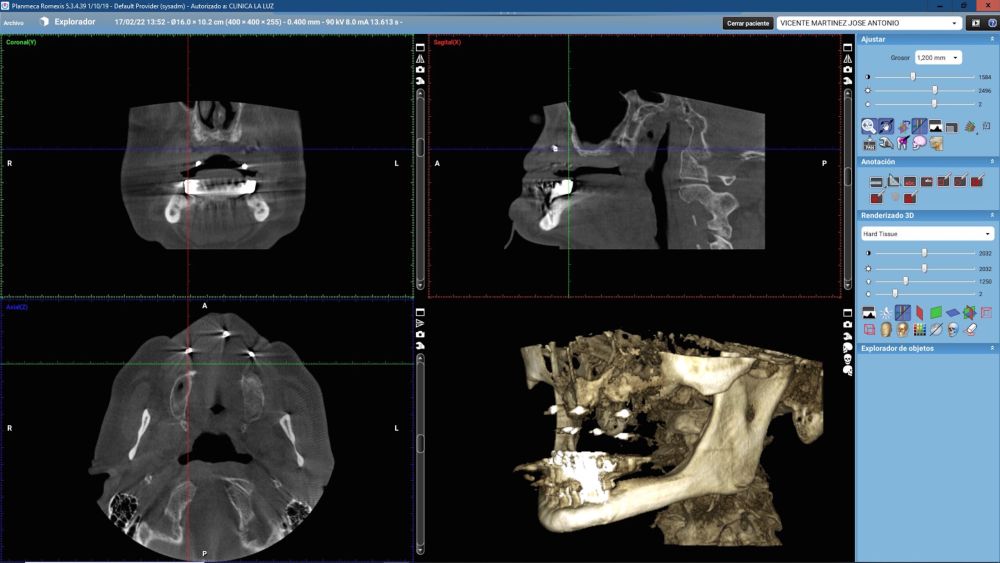
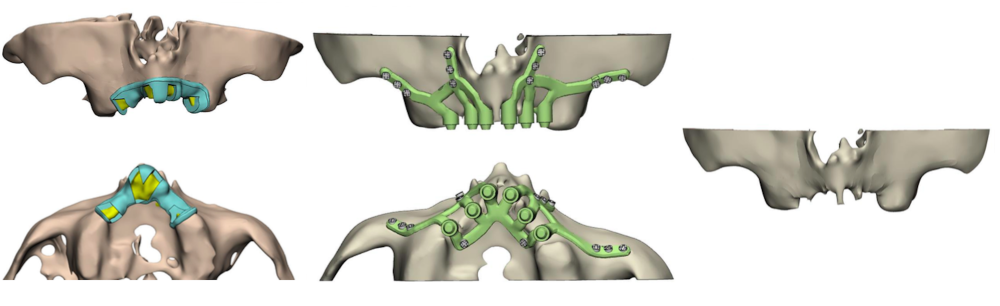
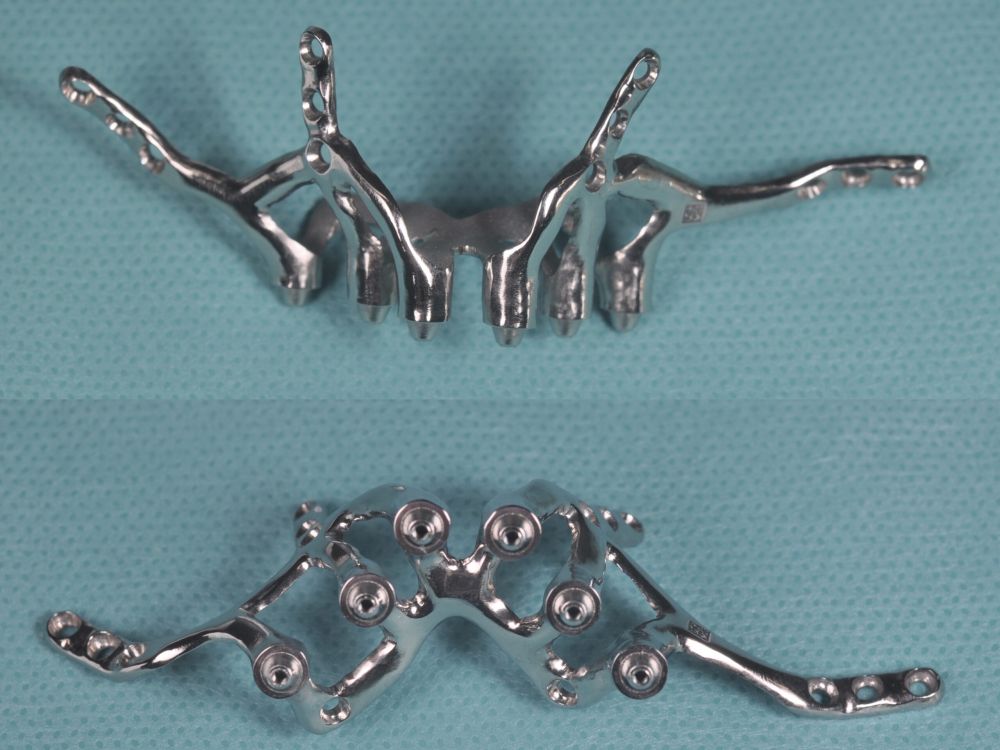
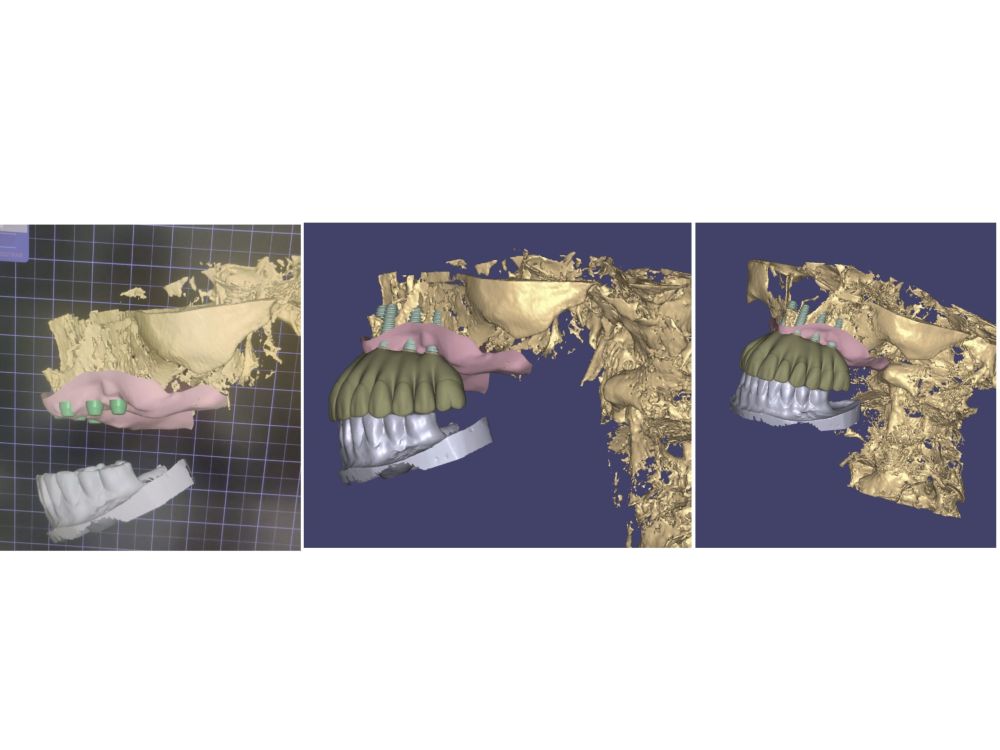
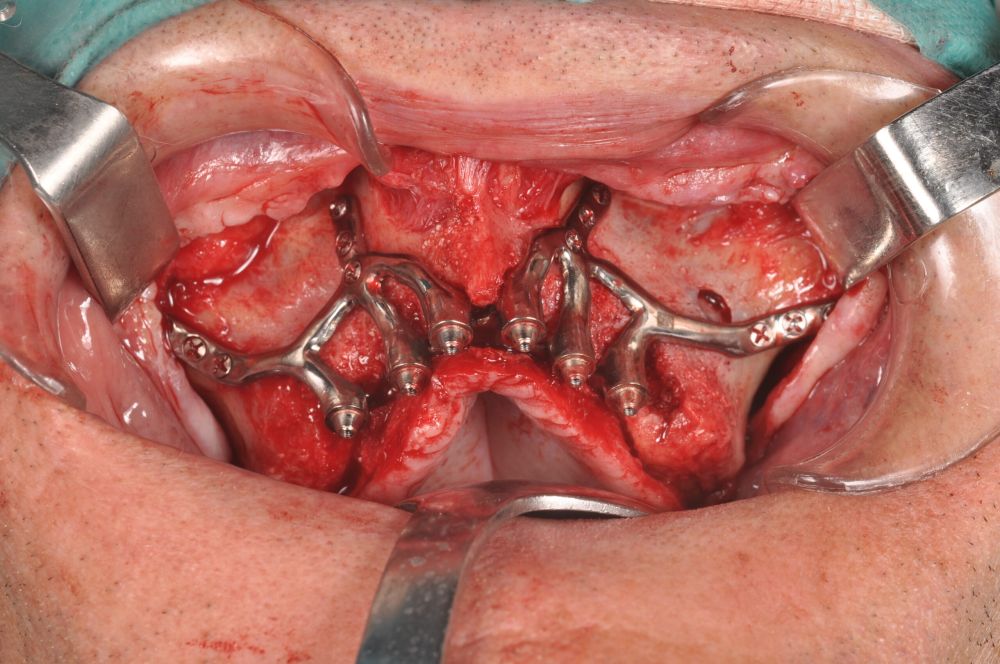
For this purpose, intraoral photographs were made and the complete prosthesis of the patient was used for the different planning tests. First, the double scanning technique was used, adding different radiopaque markers with gutta percha in the prosthesis10 (Figure 3). Then, the scanning was obtained with a conical beam computerized tomography (CBCT), (Planmeca ProMax 3D, Helsinki, Finland), both the prosthesis and the patient with his prosthesis stabilized with a silicone bite registration (Figure 4). In addition, an intraoral scan of the patient’s prosthesis was performed. From this, a personalized structure was designed subperiosteal sintered in Titanium (Ti-6-4) (Custom 3D®) with 6 Multi-Unit® type connections (Branemark, Nobel Biocare) and fixed with osteosynthesis screws in the higher density and volume areas of the malar bone and upper jaw (Figure 5 and 6). At the same time, with the STL digital test of the planning of the mesh, and with the scanning of our complete prosthesis, the laboratory technician made an implantosupported rehabilitation milled in polymethylmethacrylate (PMMA) with Multi-Unit® type titanium interfaces for immediate loading (figures 7 and 8).
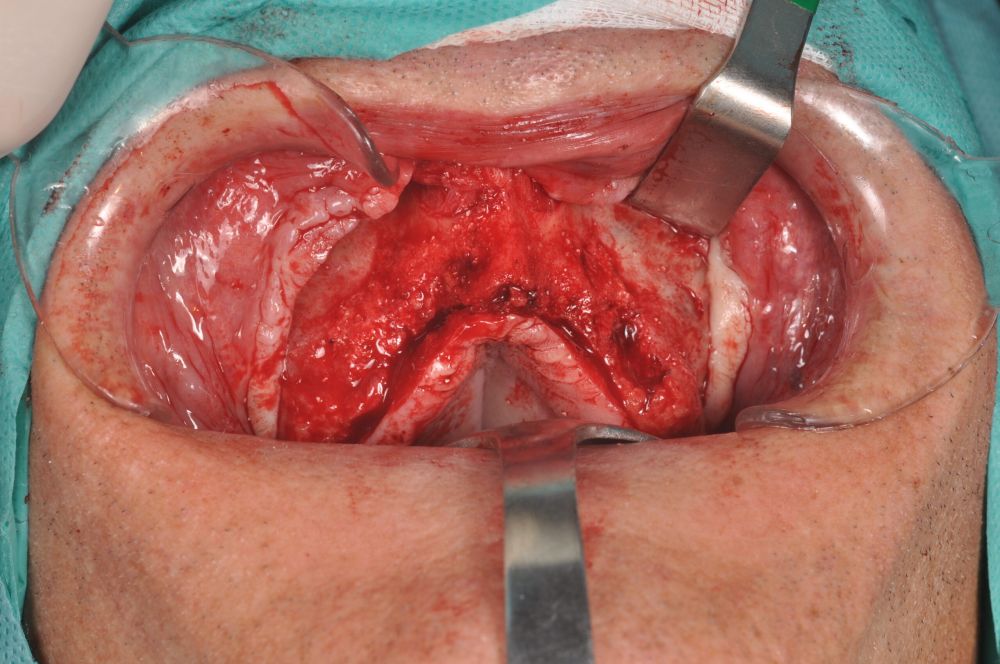
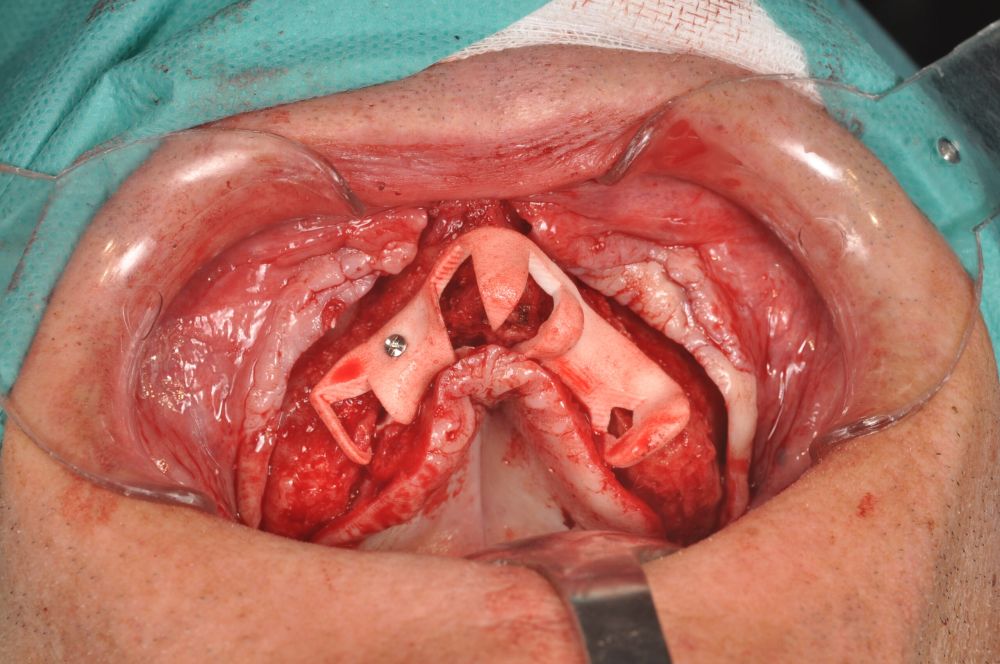
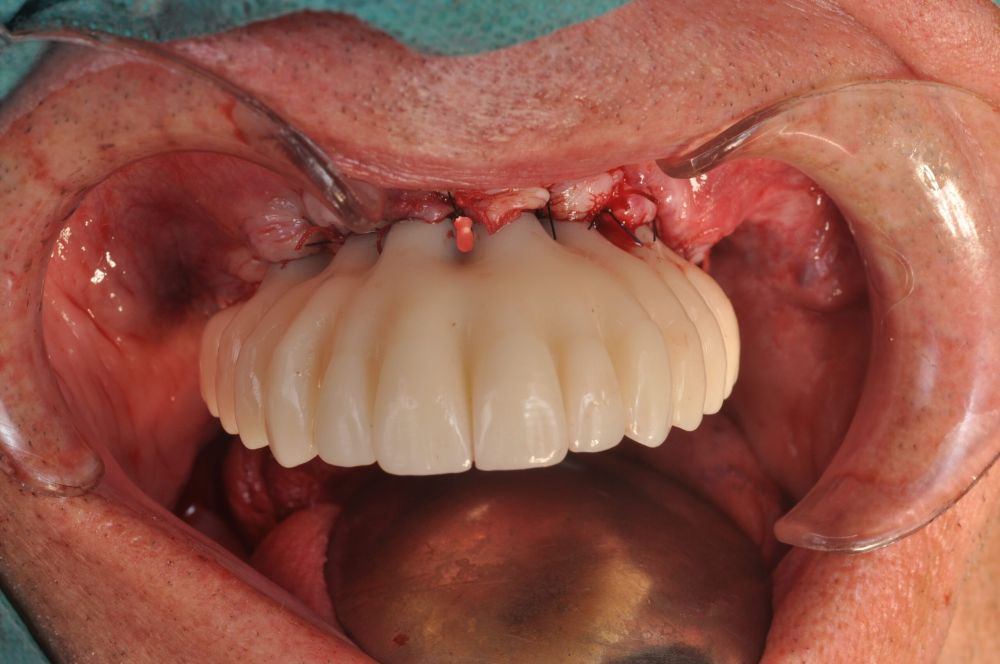
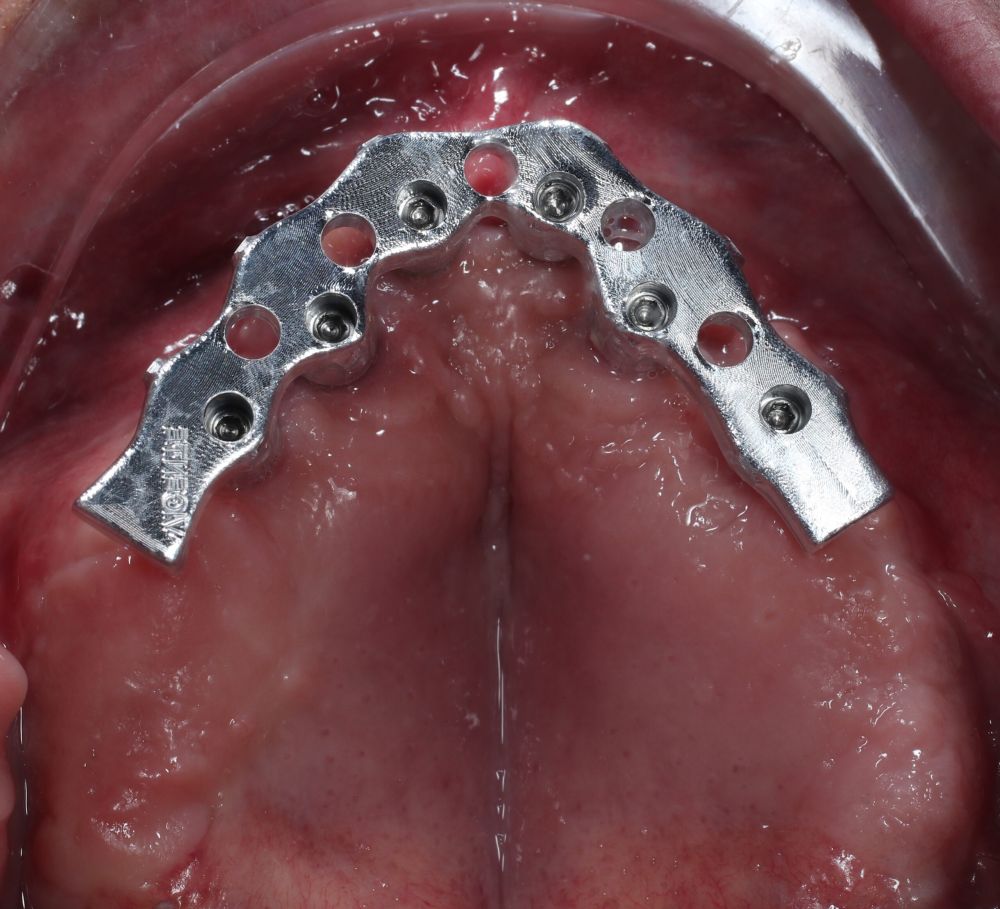
The surgical procedure was performed under general anaesthesia and nasotracheal intubation. A supracrestal incision and detachment of a maxillary flap of total thickness was made (Figures 9 and 10). The boundaries of the dissection were both infraorbital ridges, both laterally malar bodies and the anterior half of the hard palate caudally. In addition, a customized cutting guide was used so that the SI was completely in direct contact with the bone (Figure 11) and the mesh was fixed with the different 1.5 mm osteosynthesis screws in the nasal and zygomatic buttresses (KLS Martin, Freiburg, Germany) (Figure 12). The closure was performed with nonresorbable suture. Finally, the PMMA provisional rehabilitation was screwed for the immediate load, with a torque of 20 N on the implants (Figures 13-15).
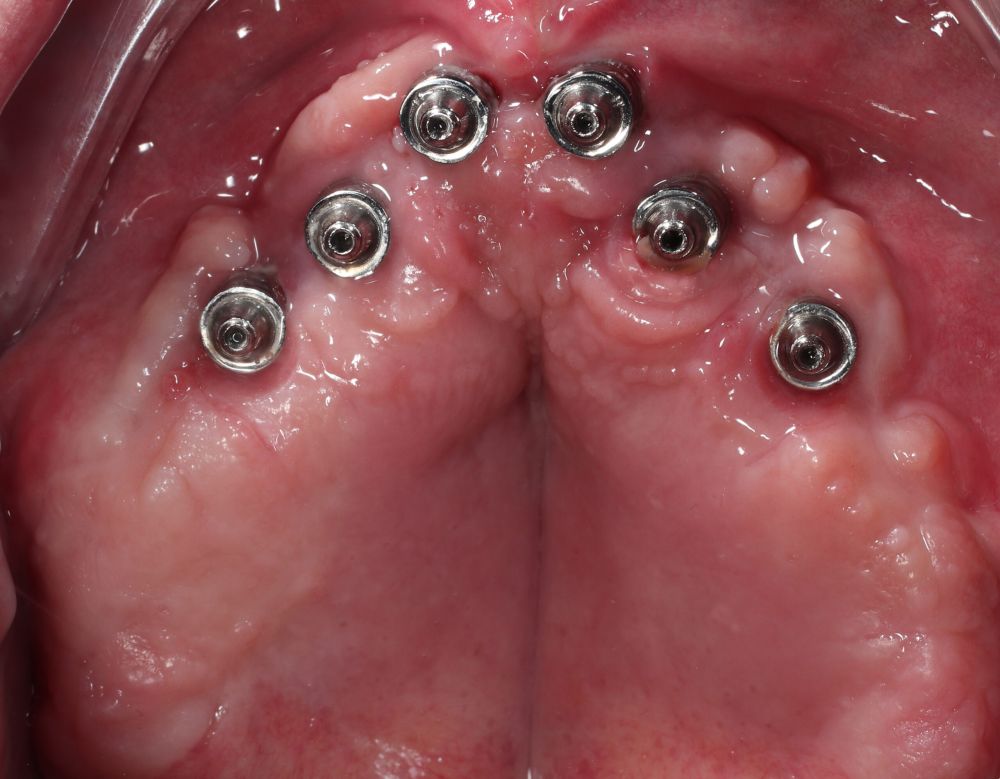
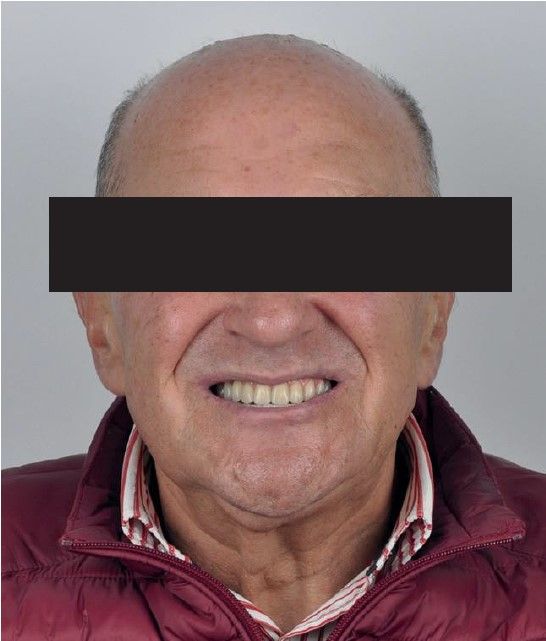
Two months later, with the soft tissues healed around the connections (Figure 16), a new intraoral scanning was made of the implants and the provisional prosthesis for future restoration. A FRI type passivity test (rigid impression splint) was manufactured with an aluminium structure to assess the correct fit on the implants (Figure 17). For implant-supported rehabilitation, a sintered structure was made in chrome-cobalt with machined bases covered with acrylic resin teeth from Bredent® (Figures 18-21).
The patient has been checked every six months this year, performing X-rays and cleaning the structure, without finding any prosthetic or periodontal complications.
Implantological rehabilitation in patients with severe maxillary atrophies has always been a challenge for the surgeon11. The progress in diagnosis and planning, the improvement in regeneration techniques and the design of materials, represent an improvement in the resolution of these complex cases. However, complications may arise in these surgeries, increasing the morbidity, time and cost of the treatment for the patient12.
The SI were widely used in the mid-50s, until the appearance of endoosseous implants, due to the ease of placement and rehabilitation13. However, the new technologies in titanium additive printing and 3D planning return to SI its role as a viable therapeutic alternative in severe maxillomandibular atrophies. The use of high-quality imaging tests and 3D planning programs allow to represent a patient’s residual bone volume with submillimetre accuracy. These data allow us to generate a virtual bone model, with which to adapt accurately the SI to the pre-existing anatomy14.
In 2009, Kusek published a clinical case of a rehabilitation on SI using CAD/CAM technology for the manufacture of a sterolythographic model in epoxy resin that was subsequently sent to the laboratory for the casting of structures15. In recent years, the additive technique of laser sintering for the manufacture of various structures in titanium and chromium-cobalt, is the one being used to process these subperiosteal implants.
In 2016, Cohen et al. published an in vitro study on the biological behaviour of SI structures produced in Ti6Al4V, using laser sintering and post-machining on different surfaces (SL)16. It demonstrated a high bone-implant contact, with a vertical growth histologically and histomorphometrically demonstrated.
In 2017, Mommaerts exposes a new design for the SI, using osteosynthesis screws fixed in the maxilla and malar zones, and various transmucosal connections are housed in the structure to screw the temporary or permanent prosthesis, using a digital protocol for this17.
The Cerea et al.18 retrospective clinical study includes the largest number of rehabilitated patients with this technique. It was performed on 70 patients with a two year follow-up. The maxilla and jaw of these patients were partially or totally rehabilitated with subperiosteal implants manufactured on laser sintered structures and a subsequent electropolishing process, making the surfaces completely smooth. The survival rate of the implants was 95.8% and the main postsurgical complications were pain, discomfort and swelling. There was an 8.9% rate of prosthetic complications.
In 2020, Mangano et al.19 published a study of 10 patients with mandibular atrophic posterior sectors. These were rehabilitated with SI manufactured on laser sintered structures and subsequent decontamination and sterilization with organic acids. Within a year, no implants had been lost and all complications were minor.
Today, SI rehabilitation has improved significantly due to the great advances in digital planning and CAD/CAM. Although more studies are needed, it is an alternative tool in cases of complex surgeries with large atrophies with the possibility, in addition, to perform an immediate load.
Srinivasan M, Meyer S, Mombelli A, Müller F. Dental implants in the elderly population: a systematic review and meta-analysis. Clin Oral Implants Res. 2017;28(8):920-930.
doi: 10.1111/clr.12898.
Lim G, Lin GH, Monje A, Chan HL, Wang HL. Wound Healing Complications Following Guided Bone Regeneration for Ridge Augmentation: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2018;33(1):41–
50. doi: 10.11607/jomi.5581.
Weiss CM, Reynolds T. A collective conference on the utilization of subperiosteal implants in implant dentistry. J Oral Implantol. 2000;26(2): 127–8.
Linkow LI, Wagner JR, Chanavaz M. Tripodal mandibular subperiosteal implant: basic sciences, operational procedures, and clinical data. J Oral Implantol. 1998;24(1):16–36.
Linkow LI. Use of a tripodal mandibular subperiosteal implant with ramus hinges for facial asymmetry. J Oral Implantol. 2000;26(2):120–3.
Van Steenberghe D, Brånemark PI, Quirynen M, De Mars G, Naert
I. The rehabilitation of oral defects by osseointegrated implants. J Clin Periodontol. 1991;18(6):488-93.
Moore DJ, Hansen PA. A descriptive 18-year retrospective review of subperiosteal implants for patients with severely atrophied edentulous mandibles. J Prosthet Dent. 2004;92(2):145-50.
Schou S, Pallesen L, Hjørting-Hansen E, Pedersen CS, Fibaek B. A 41-year history of a mandibular subperiosteal implant. Clin Oral Implants Res. 2000;11(2):171-8.
Mommaerts MY. Additively manufactured sub-periosteal jaw im-plants. Int J Oral Maxillofac Surg 2017;46:938–40.
Gillot L, Noharet R, Cannas B. Guided Surgery and Presurgical Prosthesis: Preliminary Results of 33 Fully Edentulous Maxillae Treated in Accordance with the NobelGuide Protocol. The NobelGuide® Protocol. 2010;12:e104–13.
Esposito M, Grusovin MG, Felice P, Karatzopoulos G, Worthington HV, Coulthard P. The efficacy of horizontal and vertical bone augmentation procedures for dental implants – a Cochrane systematic review. Eur J Oral Implantol. 2009;2(3):167-84.
Barone A, Ricci M, Mangano F, Covani U. Morbidity associated with iliac crest harvesting in the treatment of maxillary and mandibular atrophies: a 10-year analysis. J Oral Maxillofac Surg. 2011;69(9):2298-304.
Esposito M, Ardebili Y, Worthington HV. Interventions for replacing missing teeth: different types of dental implants. Cochrane Database Syst Rev. 2014 22;(7):CD003815.
Garrido-Martínez P, Quispe-López N, Montesdeoca-García N, Esparza- Gómez G, Cebrián-Carretero JL. Maxillary reconstruction with subperiosteal implants in a cancer patient: A one-year follow-up. J Clin Exp Dent. 2022;14(3):e293-e297.
Kusek RE. The Use of Laser Technology (Er;Cr:YSGG) and Stereolithography to Aid in the Placement of a Subperiosteal Implant: Case Study. J Oral Implantol 1 2009; 35 (1): 5–11.
Cohen, D., Cheng, A., Kahn, A. et al. Novel Osteogenic Ti-6Al-4V Device For Restoration Of Dental Function In Patients With Large Bone Deficiencies: Design, Development And Implementation. Sci Rep 6, 20493 (2016).
Mommaerts MY. Additively manufactured sub-periosteal jaw implants. Int J Oral Maxillofac Surg 2017; 46:938–40.
Cerea M, Dolcini GA. Custom- Made Direct Metal Laser Sintering Titanium Subperiosteal Implants: A Retrospective Clinical Study on 70 Patients. Biomed Res Int. 2018;
2018:5420391.
Mangano C, Bianchi A, Mangano FG, y cols. Custom-made 3D printed subperiosteal titanium implants for the prosthetic restoration of the atrophic posterior mandible of elderly patients: a case series. 3D Print Med. 2020 8;6(1):1.

Garrido Martínez, Pablo
Doctor in Odontology Universidad Complutense de Madrid (UCM).
Master Degree in Maxillofacial Prosthetics UCM. Professor of Prosthesis and Occlusion Universidad Alfonso X El Sabio (UAX). Maxillofacial Surgery and Dentistry Department Hospital La Luz, Madrid.
Montesdeoca García, Nestor
Doctor in Medicine and Surgery Universidad de Navarra. Specialist in Oral and Maxillofacial Surgery, Hospital La Paz, Madrid. Head of the Maxillofacial Surgery and Dentistry Unit, Hospital La Luz, Madrid.
Esparza Gómez, Germán
Doctor of Medicine and Surgery UCM. Specialist in Stomatology UCM. Associate Professor of Oral Medicine UCM.
Quispe López, Norberto
Doctor in Dentistry UAX. Master Degree in Periodontics and Implantology UAX. Master Degree in UAX Endodontics. Periodontology Associate Professor Universidad de Salamanca (USAL).
Cebrián Carretero, José Luis
Doctor in Medicine and Surgery UAM. Degree in Dentistry UE. Specialist in Oral and Maxillofacial Surgery, Hospital La Paz, Madrid. Head of Services of Oral and Maxillofacial Surgery, Hospital La Paz, Madrid. Head of Services of Maxillofacial Surgery and Dentistry, Hospital La Luz, Madrid.