Original article
Published in spanish Científica Dental Vol. 17. Nº 2. 2020 www.cientificadental.es
Craniocervical position characteristics for different occlusions in developing patients: Craniocervical relationship and occlusion
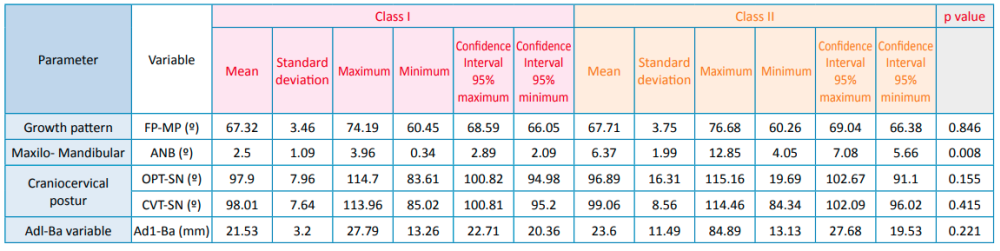
Currently, the relationship between occlusion and posture arouses great scientific interest, especially during the establishment of a multidisciplinary treatment. However, the diversity of studies refers mostly to the adult population and there is no common agreement among the different investigations. Based on this, we aimed to study the craniocervical position in different occlusions in the developing pediatric population. Through a crosssectional design, 64 pediatric patients with complete clinical history and highquality lateral skull radiographs were selected. The variables analyzed by ImageJ™ and Nemoceph™ software’s were FP-MP, ANB angle, OPT-SN, CVT-SN and Ad1-Ba. Descriptive and comparative statistical analysis were carried out with IBM SPSS Statistics™ software, subsequently finding intra-examiner agreement. P-values obtained for each of these variables were 0.846 for FP-MP, 0.008 for ANB angle, 0.155 for OPT-SN, 0.415 for CVT-SN, and 0.221 for CVT-SN. Based on these results, we believe that the craniofacial position in the different occlusions could be determined by the fact that the development has not yet been completed.
The relationship between dentistry and posture has been a constant source of interest and research in recent decades1-3. Malocclusion is not only the result of the action of genetic and environmental factors, but also postural ones. Cervical alterations such as fusions and posterior arch deficiencies can be observed in patients with occlusal alterations2 .
However, there are several systematic reviews that demonstrate a lack of reliable scientific information on this relationship, especially in developing patients. This confusion is partly due to the great variety of methodological approaches and errors in studies carried out4-7.
Authors such as Aranitasi et al,2 affirm that nonsyndromic patients with skeletal class II or III have a high prevalence of fusion between cervical vertebrae. According to Lippold et al,8 there are associations between occlusion anomalies and scoliosis in preschool populations. Solow and Sonnesen9 observed a clear association pattern between crowding of more than 2 mm and craniocervical posture in paediatric patients.
For D’Attilio et al,10 children with skeletal class III may have a significantly lower angle of cervical lordosis compared to those of skeletal classes I and II; with a significantly greater extension of the head over the spine in class II malocclusions, when compared with skeletal classes I and III.
According to Gogola et al,11 infants with defective postures have more marked malocclusions than those with correct body posture.
Another aspect to take into account in this area is the importance of the airway. Therefore, when evaluating the nasal pathway and oropharyngeal volumes in children and with different dentofacial skeletal patterns, it was observed that the position of the mandible with respect to the cranial base had an effect on the airway volume12. For Kim et al,13 head posture in children and adolescents is associated with different craniofacial dimensions, thereby determining an aetiological respiratory component in cases with open bite.
Sidlauskiene et al,14 analysed occlusion and general body posture in children, as well as nasopharyngeal pathology, such as deviations in the nasal septum, hypertrophy of adenoids, tonsils and allergic rhinitis. They found a statistically significant relationship between the presence of a kyphotic posture and a reduction in the SNB angle, representing the sagittal position of the jaw; and a statistically significant association between kyphotic posture and nasopharyngeal obstruction.
Rocha et al,3 when evaluating the mode of respiration, occlusion and posture parameters in children and adolescents, observed a lower position of the hyoid bone with respect to the plane of the jaw in some study groups with oral respiration. For Silvestrini et al,15 postural, orthoptic, osteopathic and occlusion variables were often clinically associated in children; therefore, all these disorders seem to require a multidisciplinary medical approach for their treatment.
These aforementioned precedents demonstrate that the relationship between occlusion and posture has been a continuing source of interest for all professionals in the provision of health care over the last decades. According to Perinetti16, this importance lies in the fact that dental malocclusion is very highly prevalent among children; therefore, its potential negative effects on body posture could provide other indications for orthodontic treatments.
The lack of consensus among different investigations and the few studies in developing patients invites us to study the craniocervical position in different occlusions in this population.
After obtaining informed consent and the approval of the Clinical Research Ethics Committee, a crosssectional study was carried out on paediatric patients with the following selection criteria: being 6-years old with a complete medical history and lateral skull x-rays, non-syndromic, without craniofacial malformations or a surgical history of the upper airway, who had not received orthodontic treatments and with lateral skull radiographs without distortion, enlargement, superposition of structures or difficulty in identifying and recording anatomical points. No contact was made with the sample for this study, with only the medical history data and radiographic records being reviewed.
The growth predisposition pattern was quantitatively determined using the FP-MP cephalometric parameter, defined as the angle formed between the facial and mandibular planes. Skeletal class was diagnosed through Steiner’s analysis using the ANB angle measurement.
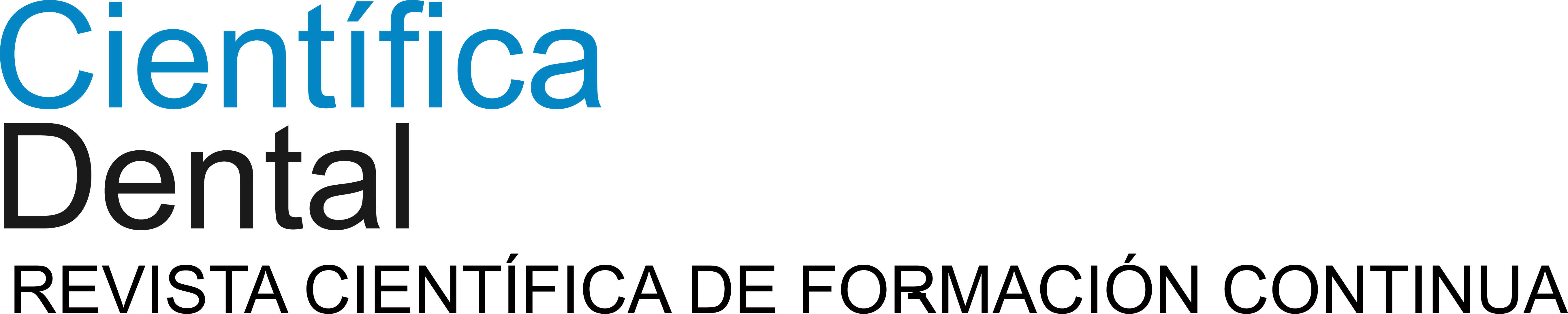
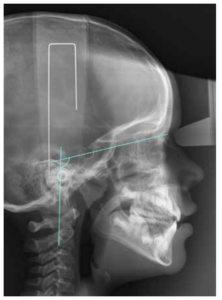
Craniocervical posture was assessed via the variables OPT-SN, which refer to the angle formed by SN and the line that runs through the most postero-superior and postero-inferior point of the odontoid process (Figure 1).
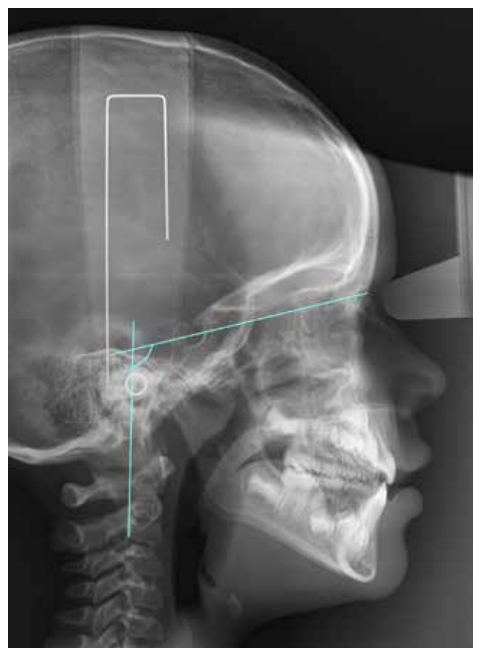
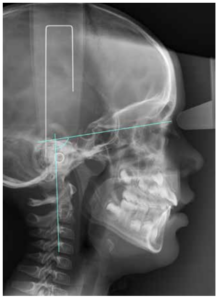
Another variable studied was the CVT-SN, which is the angle formed between SN and the line that runs through the postero-superior and postero-inferior points of the four cervical vertebrae (Figure 2).
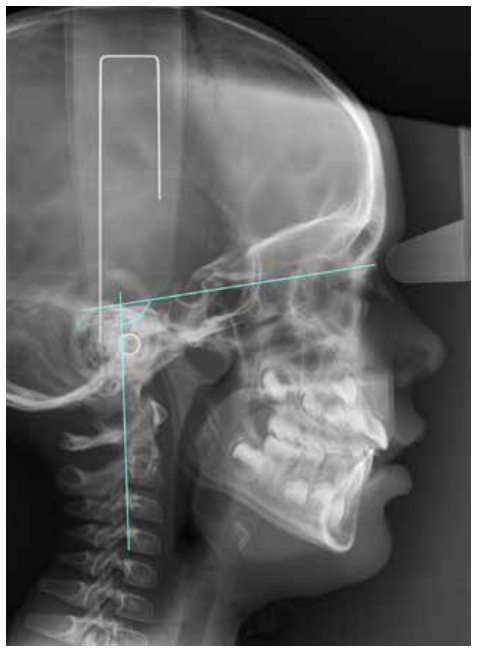
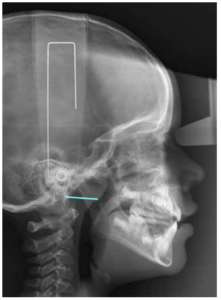
Finally, the distance was measured between the intersection point of the posterior pharyngeal wall and the line formed between the posterior nasal spine along with the basion (Ad1-Ba), refer to Figure 3.
All these study variables were obtained after calibration of the radiographs, using the length of the metal rods as a reference point, after locating and establishing the structural reference points; by using ImageJ™ and Nemoceph™ software. Finally, the results of the variables were tabulated for each of the selected subjects.
The measurement for each radiographic record took around 40 minutes on average. To detect any errors in intra-examiner identification, 10% of the records studied were randomly selected and measured 2 weeks later.
The data were analysed by descriptive and comparative statistical methods using the IBM SPSS™ program. The quantitative variables were described using the mean and standard deviation, and the difference in means was analysed by using either Student’s t test, for variables that had a normal distribution, or the Mann Whitney U test, for those that did not; with p < 0.05.
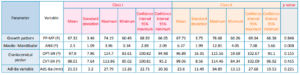
Data from 64 patients was collected, of which 31 (48%) had Steiner cephalometric values of ANB class I and 33 (52%) were class II. The table shows the results obtained in relation to the study parameters. Of all the variables measured, there was only significance for the values relative to ANB (p = 0.008). Intra-examiner agreement was calculated using the Kappa index and was 100%.
Studies reviewed in the literature with comparable samples were Rocha et al,3 Solow and Sonnesen9 , D’Attilio et al,10 Arntsen and Sonnesen17, Kim et al,13 and Gogola et al,11 since the subjects in these studies were of a similar age to those in our study.
For sample size, Perinetti, and Tardieu et al,18 had a smaller sample than ours, 20 and 26 subjects, respectively; Castro-Silva et al,19 had a similar sample size to ours, 60 participants; while Arntsen and Sonnesen17, Ei and Palomo12, Silvestrini et al,15 Kim et al,13 Gogola et al,11 Sidlauskas14, Solow and Sonnesen9 , D’Attilio et al,10 and Rocha et al,3 had larger samples than ours: ranging from 94 in Sidlauskas14 up to 605 subjects in Silvestrini et al.15
Although the majority of the posture and occlusion studies shared a common feature with ours in being cross-sectional studies, the methodology, variables and approach given in the objectives were different in all.
The D’Attiiio et al study10 investigated the differences between cervical posture and skeletal classes and, although we shared the software used in this study, we did not agree with the posture parameters.
Perinetti16 determined this relationship through posturography. This research was different from ours; not only in the sample study variables and age, but also in being designed to determine a dynamic relationship between both variables.
However, Tardieu et al,18 investigated the influence of an occlusion disturbance on posture control according to the difficulty of the requested task. In our study there was no direct contact with patients and this task was not required.
Arntsen and Sonnesen17 associated both study parameters by examining the cervical column and craniofacial morphoiogy in subjects with class II malocclusion and overjet; they also used different software to ours (TIOPS 2005™). Meanwhile, Silvestrini et al,15 added parameters such as ocular convergence to the studied relationship.
Kim et al,13 designed a study where the morphology of the cervical spine was described for the first time in children and adolescents with open bite. Our research did not take into account the occlusion alteration in the vertical plane and had different study variables. Gogoia et al,11 used different occlusion parameters as well as an approach to the posture of the craniocervical area.
Sidiauskas14 investigated the relationship between occlusion and the patient’s general body posture, also including nasopharyngeal pathology, such as deviations in the nasal septum, hypertrophy of the adenoids and tonsils, and allergic rhinitis. However, in our study neither the general body posture nor nasal pathology was evaluated.
Rocha et al,3 included oral or nasal breathing mode, in addition to the occlusion and posture relationship, and was the most similar study to ours in terms of variables; they used the Ortho TP™ orthodontic software and an airflow sensor for the digital e-Health Platform™. In subjects aged 7-9 years, they also found no statistically significant results in relation to posture a similitude with us. There is some similarity between the two in relation to some descriptive results. The values corresponding to variable FP-MP, regarding the facial growth pattern, were 66.81 and 67.03 for group I in the Rocha et al study3 , while they were 67.3 and 67.1 for classes I and II, respectively, in our study. Their ANB parameters were 2.06 and 4.25, while in our study they were 2.49 for class I and 6.37 for class II.
The craniocervical parameters in both occlusions lacked statistical significance; thus a larger sample size study is required. Also, perhaps the young age of the population meant that this relationship was not so obvious.
We would like to thank the company Nemotec for providing the Nemoceph™ orthodontic software and all its technical support free of charge for this study.
Souza D, Martinelli E. A longitudinal evaluation of the skeletal profile of treated and untreated skeletal class II individuals. Angle Orthod 2005;75 (1): 7.
Aranitasi L, Tarazona B, Zamora N, Gandía JL, Paredes V. Influence of skeletal class in the morphology of cervical vertebrae: A study using cone beam computed tomography. Angle Orthod 2017;87(1):131.
Chambi-Rocha A, Cabrera-Domínguez ME, Domínguez-Reyes A. Breathing mode influence on craniofacial development and head posture. J Pediatr 2018; 94(2):123–130.
Amat P. Occlusion, orthodontics and posture: are there evidences? The example of scoliosis. Int J Stomatol Occlusion Med 2009;2(1):2–10.
Hanke BA, Motschall E, Türp JC. Association between orthopedic and dental findings: what level of evidence is available? J Orofac Orthop Fortschritte Kieferorthopädie 2007; 68 (2): 91–107.
Michelotti A, Buonocore G, Manzo P, Pellegrino G, Farella M. Dental occlusion and posture: an overview. Prog Orthod 2011;12(1): 53–58.
Neiva PD, Kirkwood RN, Mendes PL, Zabjek K, Becker HG, Mathur S. Postural disorders in mouth breathing children: a systematic review. Braz J Phys Ther 2018;22(1):7-19.
Lippold C, van den Bos L, Hohoff A, Danesh G, Ehmer U. Interdisciplinary study of orthopedic and orthodontic findings in pre-school infants. J Orofac Orthop Fortschritte Kieferorthopädie 2003; 64(5): 330–340.
Solow B, Sonnesen L. Head posture and malocclusions. Eur J Orthod 1998;20(6):685–93.
D’Attilio M, Caputi S, Epifania E, Festa F, Tecco S. Evaluation of cervical posture of children in skeletal class I, II, and III. CRANIO® 2005;23(3): 219–228.
Gogola A. Assessment of connection between the bite plane and body posture in children and teenagers. Develpmental Period Med 2014;18 (4):453–458.
El H, Palomo JM. Airway volume for different dentofacial skeletal patterns. Am J Orthod Dentofacial Orthop 2011; 139 (6): e511–521.
Kim P, Sarauw MT, Sonnesen L. Cervical vertebral column morphology and head posture in preorthodontic patients with anterior open bite. Am J Orthod Dentofacial Orthop 2014; 145 (3): 359–66.
Šidlauskas M. Relationships between malocclusion, body posture, and nasopharyngeal pathology in pre-orthodontic children. Med Sci Monit 2015; 21:1765–1773.
Silvestrini-Biavati A, Migliorati M, Demarziani E, Tecco S, Silvestrini-Biavati P, Polimeni A, y cols. Clinical association between teeth malocclusions, wrong posture and ocular convergence disorders: an epidemiological investigation on primary school children. BMC Pediatr 2013;13(1).
Perinetti G. Dental occlusion and body posture: No detectable correlation. Gait Posture 2006; 24(2):165–168.
Arntsen T, Sonnesen L. Cervical vertebral column morphology related to craniofacial morphology and head posture in preorthodontic children with Class II malocclusion andhorizontal maxillary overjet. Am J Orthod Dentofacial Orthop 2011; 140 (1): e1–7.
Tardieu C, Dumitrescu M, Giraudeau A, Blanc J-L, Cheynet F, Borel L. Dental occlusion and postural control in adults. Neurosci Lett 2009; 450 (2): 221–224.
Castro-Silva L, Monnazzi MS, Spin-Neto R, Moraes M, Miranda S, Real Gabrielli MF, y cols. Cone-beam evaluation of pharyngeal airway space in class I, II, and III patients. Oral Surg Oral Med Oral Pathol Oral Radiol 2015; 120 (6): 679– 683.
Kim Y-J, Hong J-S, Hwang Y-I, Park Y-H. Three-dimensional analysis of pharyngeal airway in preadolescent children with different anteroposterior skeletal patterns. Am J Orthod Dentofacial Orthop 2010; 137(3): 306.e1-306.e11.

Reichard Monefeldt, Guillermo
Graduate in Dentistry, European University of Madrid. Master in Dental Science, Complutense University of Madrid. Master in Pediatric Dentistry, Alfonso X El Sabio University.
Diéguez Pérez, Montserrat
Doctor in Dentistry. Complutense University of Madrid. European University of Madrid.