Clinical case
Published in spanish Científica Dental Vol. 19. Nº 1. 2022 www.cientificadental.es
Upper third molar autotransplant to replace a superior first molar: about a clinical case
Introduction: The development of dental implants has led to lower frequency of autotransplants, despite their high success rates and being a therapeutic alternative that allows the realization of natural, functional and aesthetic rehabilitations.
Clinical case: we present the case of a 28-year-old male who came for consultation due to the presence of some radicular remains located on
the left upper first molar. A dental autotransplant was carried out, the donor tooth being the third upper left molar, which was transplanted to the alveolus of the first molar, showing good clinical and diagnostic evolution.
Discussion: There are different therapeutic alternatives to replace
missing teeth, within which autotransplants are found, with high success rates in teeth with open and closed apex. The most frequently transplanted teeth are the third molars, as shown in the present case, suggesting as one more option, that professionals and patients should take into account.
Conclusions: Although autotransplants have more limited indications, they have a lower cost for patients, and a simpler restoration for the professional. In addition, they sustain micromovements, achieving occlusion harmony in relation to the adjacent teeth, presenting a high success rate.
The most common therapeutic options for restoring missing teeth are fixed dental supported prosthesis, dental implants, removable prosthesis, dental
autotransplants and orthodontic treatment for gaps closure1,2. However, due to the development of dental implants3, autotransplants, although an effective alternative, are not a very popular treatment1,2, although they are the only alternative that allows a natural, functional and aesthetic rehabilitation4.
An autotransplant is defined as the transplantation of a retained or erupted tooth from its original position in the mouth to an alveolus where an extraction is performed or to surgically prepared localization in the same person4-6.
The indications for autotransplants are patients treated during puberty periods, patients with non-restorative teeth requiring extraction, and that have a donor tooth, when the intentional re-implant is prescribed7 due to premature or traumatic loss of a tooth, loss of teeth due to tumours or congenital absence of teeth8.
It is an alternative particularly applicable to teething paediatric patients, where other surgical options are not indicated. In this sense, teeth autotransplants with immature apex are more favourable than those performed with closed apex2, due to pulpal revascularization and a continuous root development, with a success rate of 95%9. The autotransplant of immature teeth also presents advantages such as proprioception, pulpal revascularization and root development10.
On the other hand, autotransplant of teeth with closed apex can be successful if a duct treatment is performed after the procedure10, since revascularization is less likely to occur and, in addition, it prevents both the appearance of periapical lesions or infections as root resorptions11. Only a 15% revascularization of teeth with closed apex are achieved after the transplant, compared to 96% of teeth with open apex6.
In this regard, satisfactory results have also been obtained in adult patients8, with survival rates of 74-100%, varying according to the transplanted tooth and the follow-up period7; Boschini et al.12 reported survival rates of 95% and success rates of 80% after a 10 years follow-up. The systematic review and metaanalysis of Machado et al.1 obtained a survival rate of 81% in transplanted teeth, with a minimum of a 6 years follow-up.
Therefore, due to the high success rates described in the literature, the objective of this clinical case is to evaluate clinically and radiographically the performance of an autotransplant with a closed apex, to replace a left upper first molar, as a therapeutic alternative to an implant placement in an adult patient.
We present a clinical case of a 28-year-old male who presented severe pain in the second quadrant, associated with the presence of root remains located in the first left upper molar (2.6).
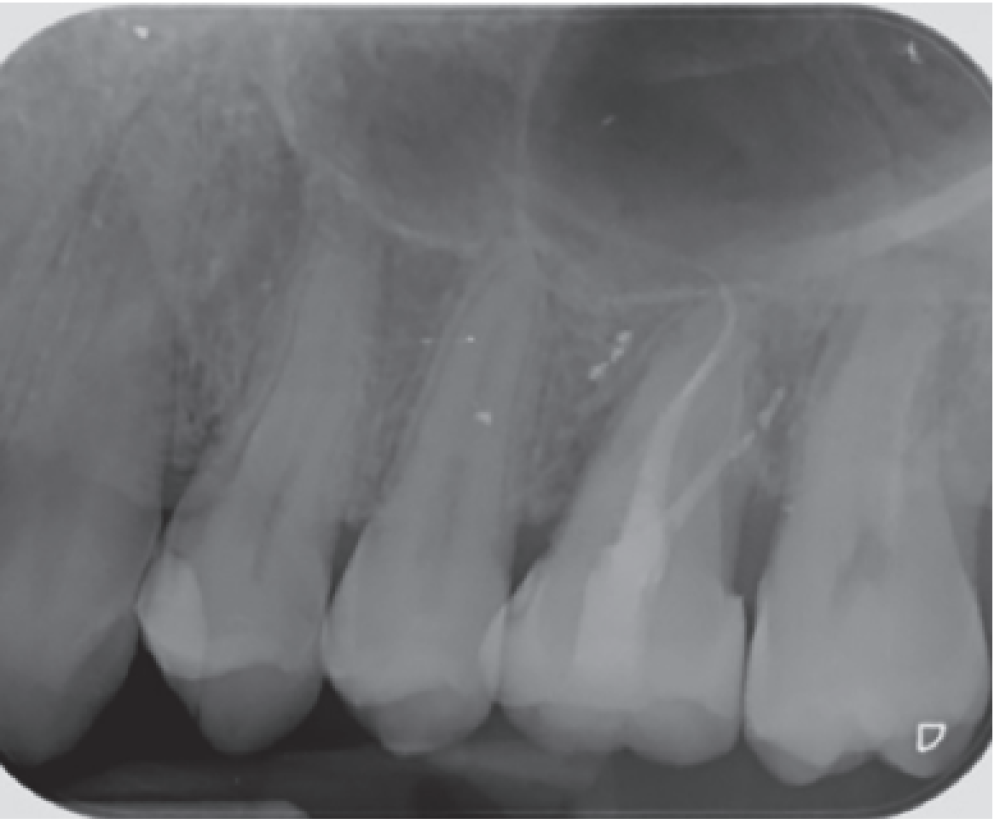
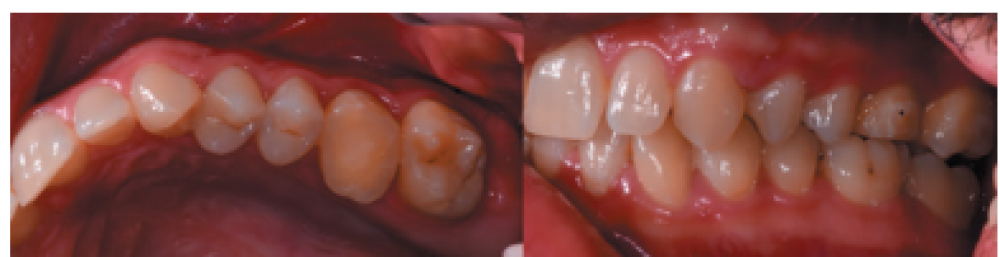
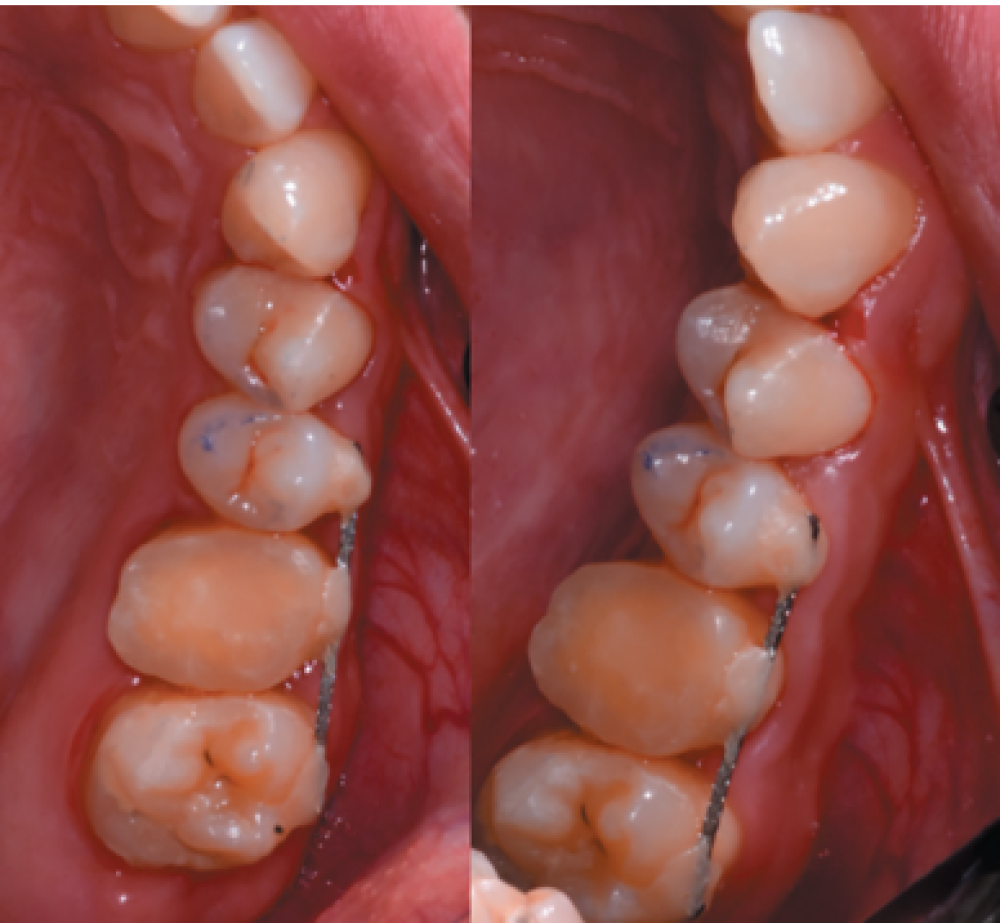
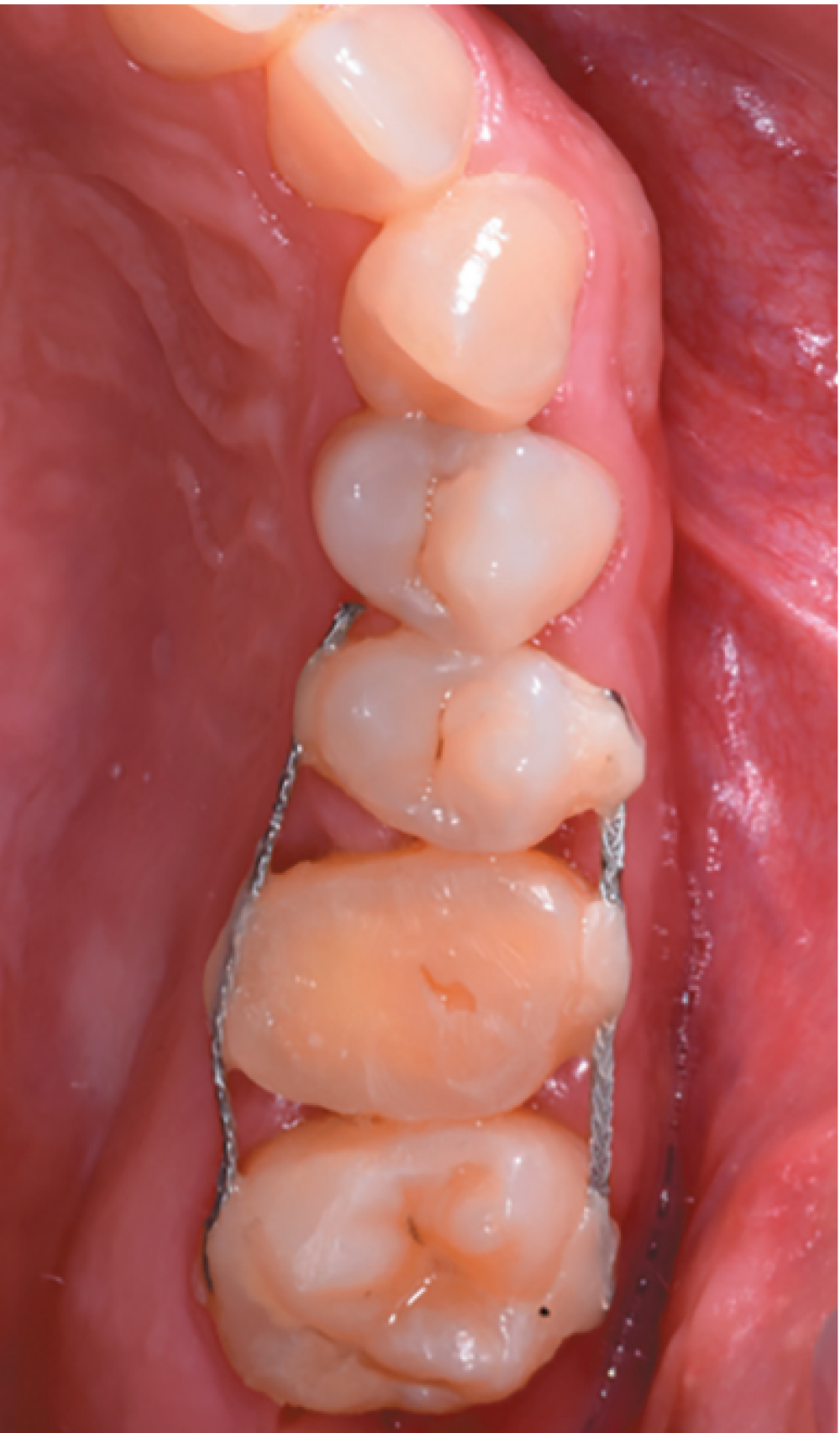
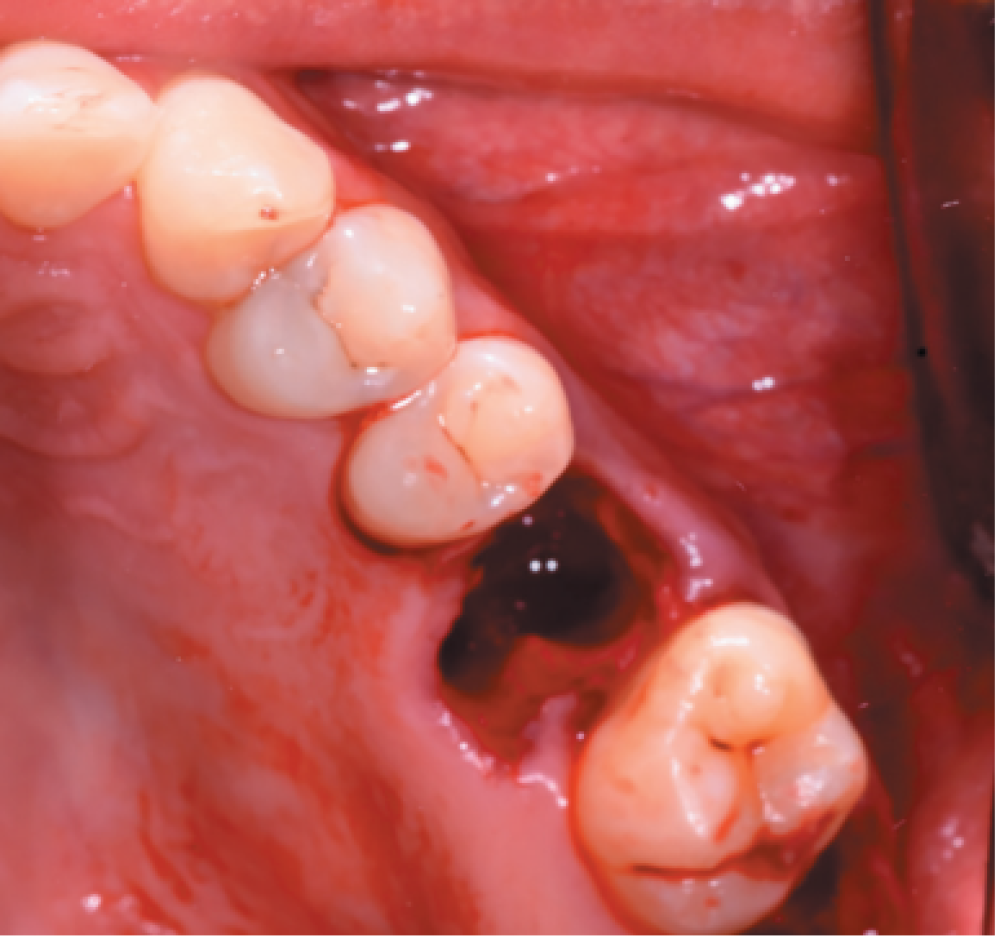
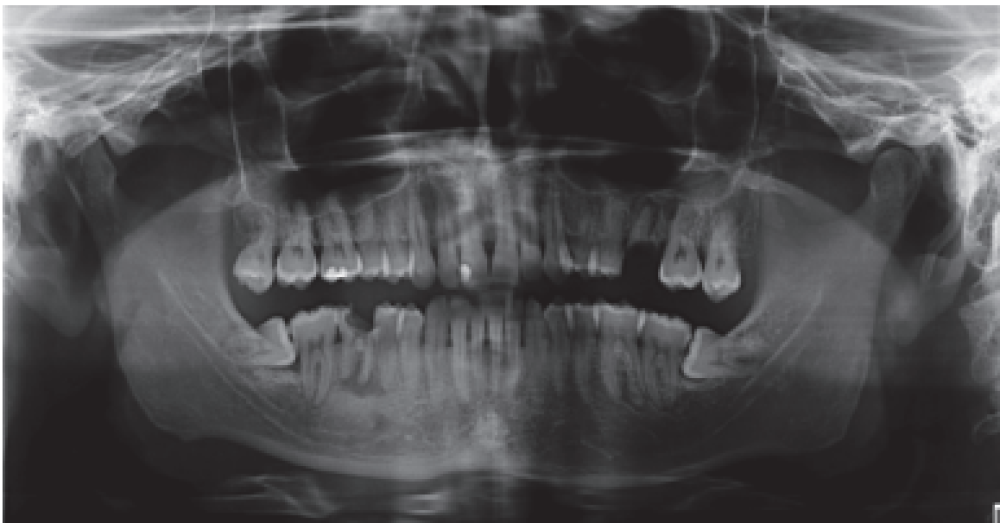
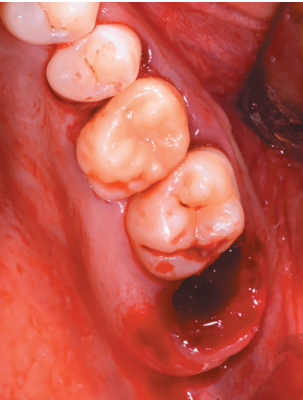
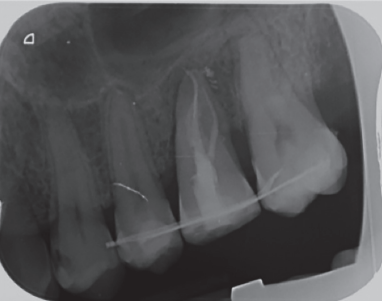
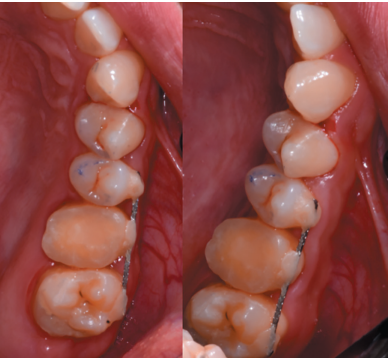
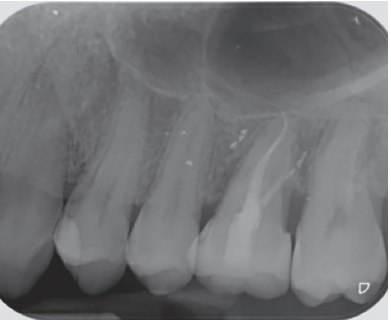
There were no medical-surgical antecedents of interest in his medical history, without known drug allergies or unhealthy habits. No relevant data was found on the extra oral examination. In the intraoral examination, non-restorable teeth were seen in the 2.6 and 4.6 position and the presence of retained lower third molars. (Figures 1 and 2).
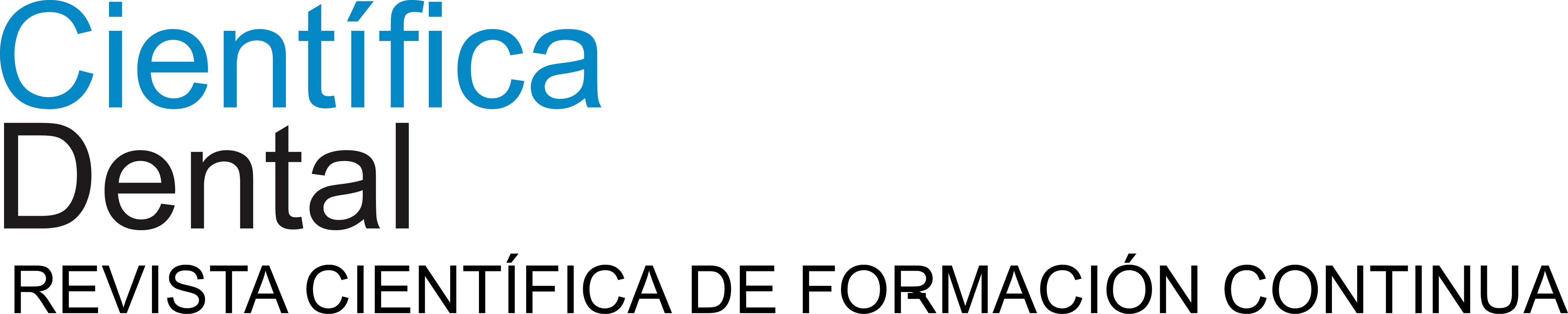
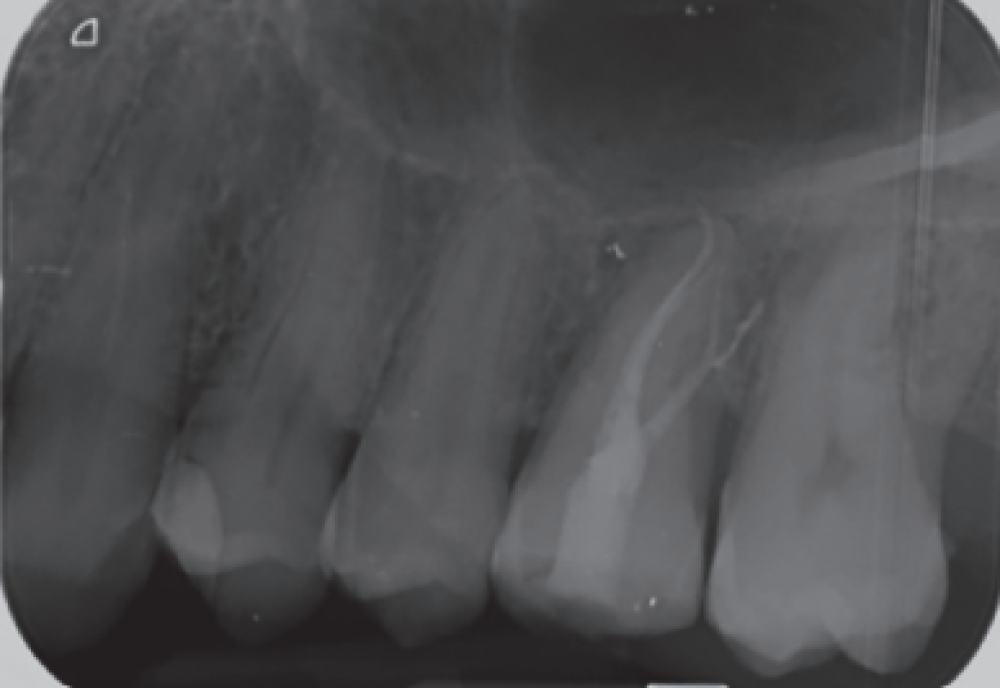
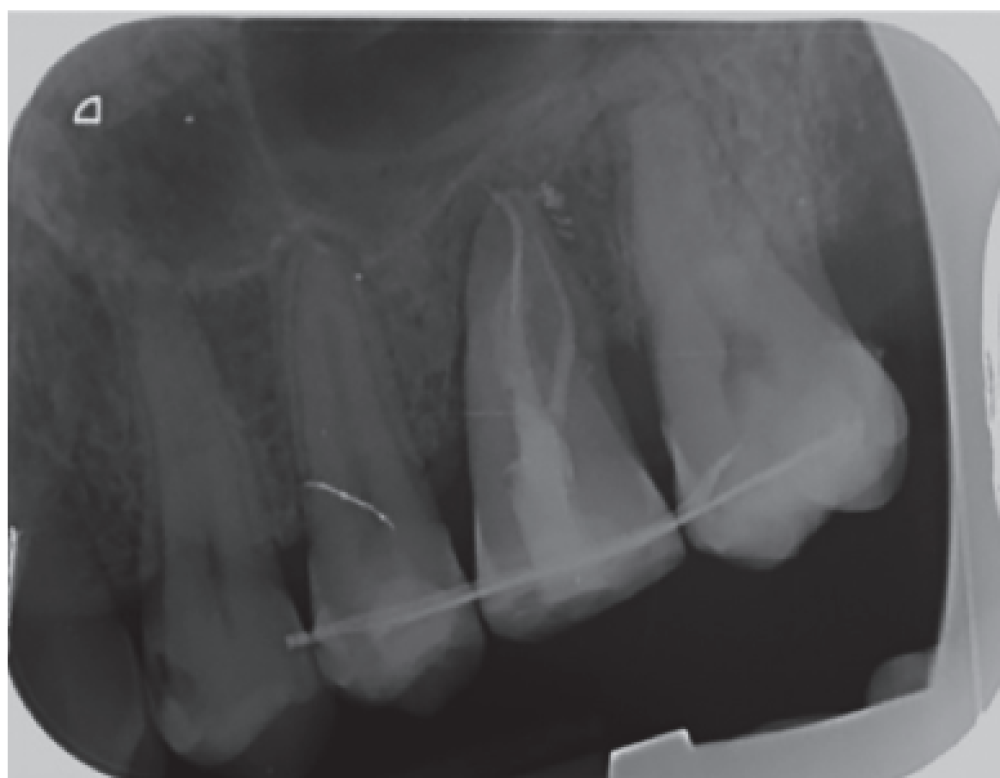
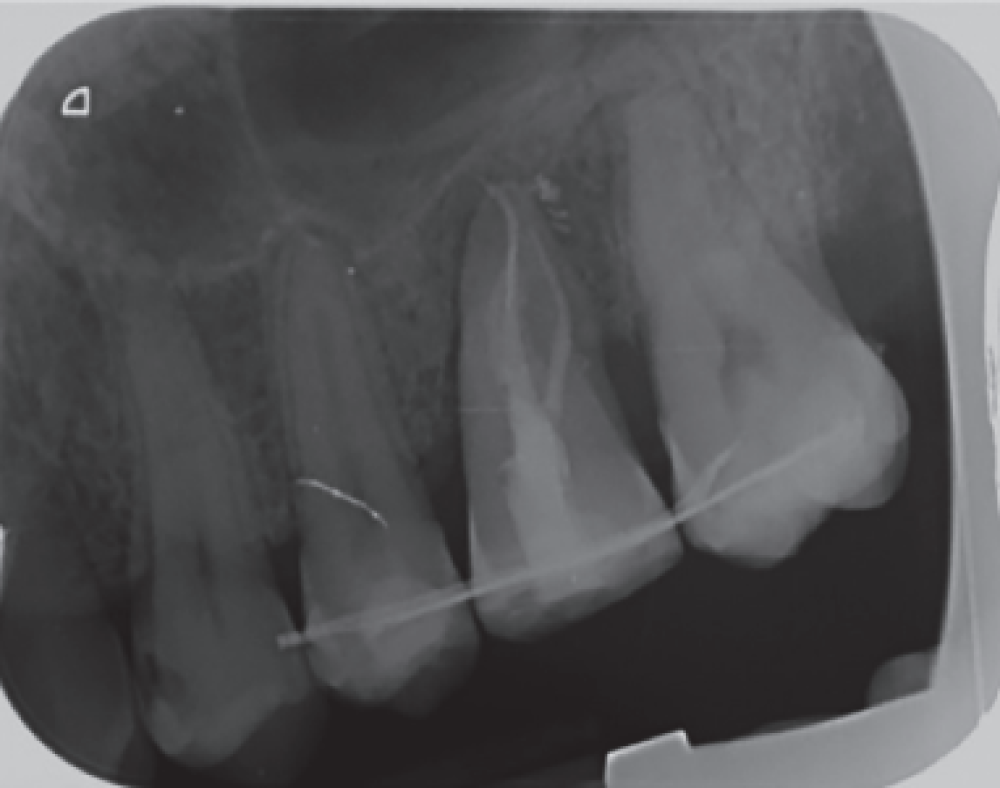
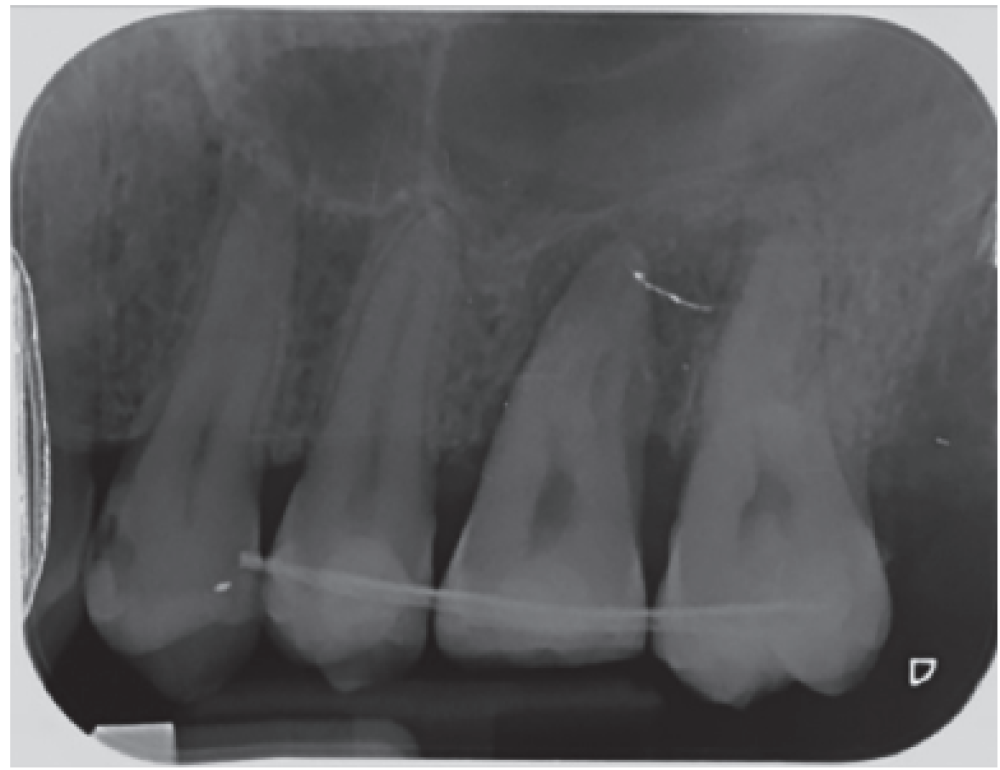
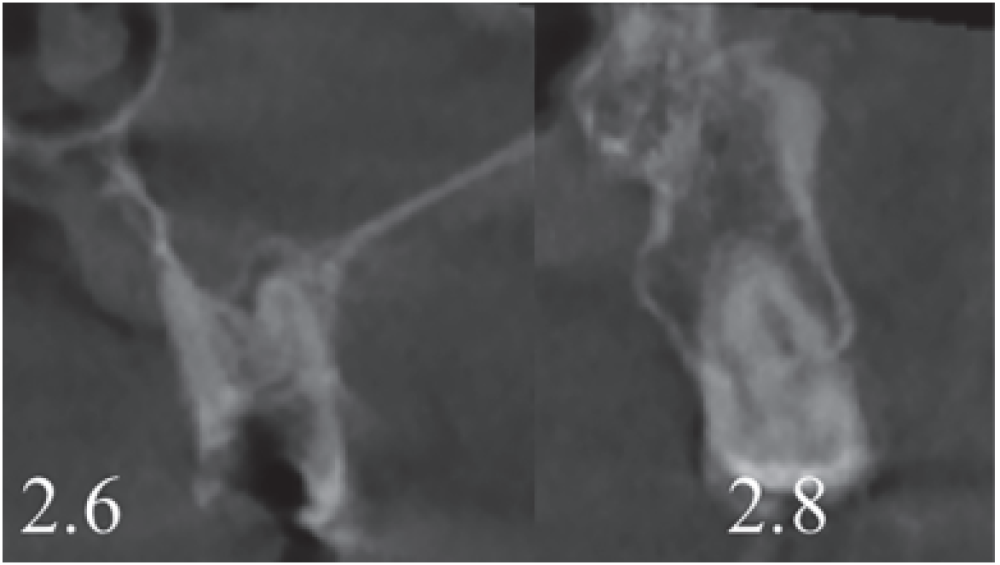
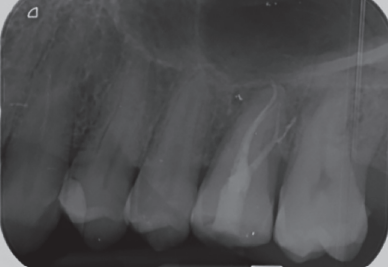
In the radiograph examination, through a panoramic radiograph, both lower third molars were seen retained in horizontal position (Figure 3), and apical radiolucent images in positions of 2.6 and 4.6. The cone beam scan evaluated the root morphology of the left upper third molar and the size of the apical radiolucent lesion of the left upper first molar (Figure 4), necessary data to assess the degree of adaptation of the donor tooth in the recipient bed.
The extraction of 4.6 and 2.6 and the curettage of the apical processes were planned, and the autotransplant of the left upper third molar (2.8) to sustain the 2.6 (Figure 5) was suggested to the patient.


associated with the root remains of 2.6 and the conical root of 2.8 are seen.

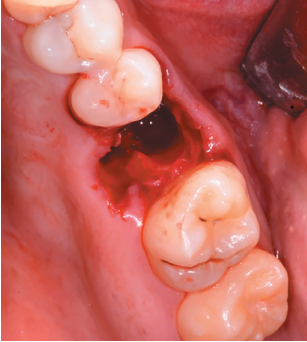
Aft er obtaining the informed consent, an anaestheti c block was performed using Arti caine 4% with Epinephrine 1:100,000 (UltracaineTM, Normon SL, Madrid, Spain) of the posterior and middle superior alveolar nerve, and anterior palati ne. An atraumati c extraction of the root remains of the 2.6 and the
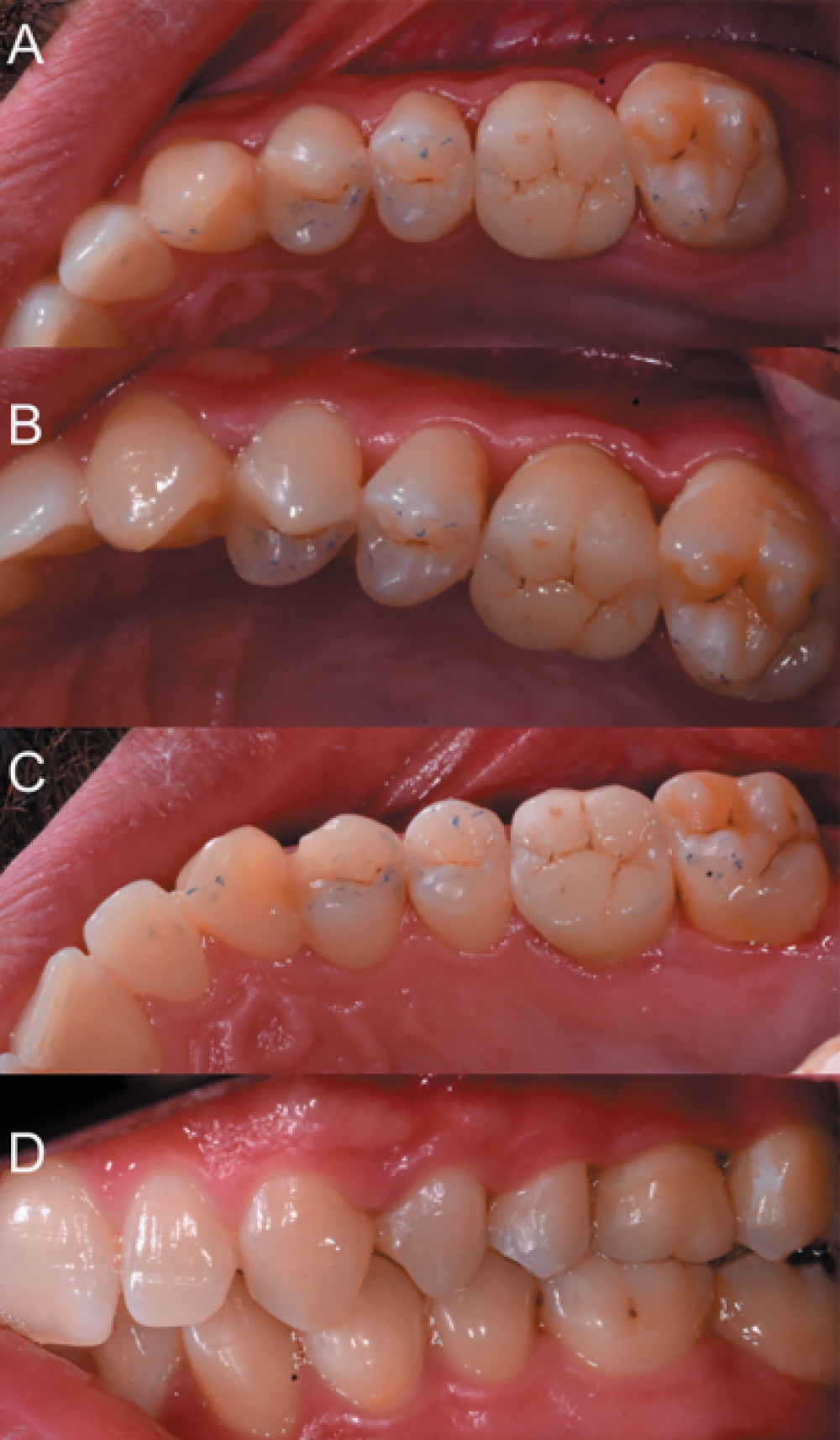
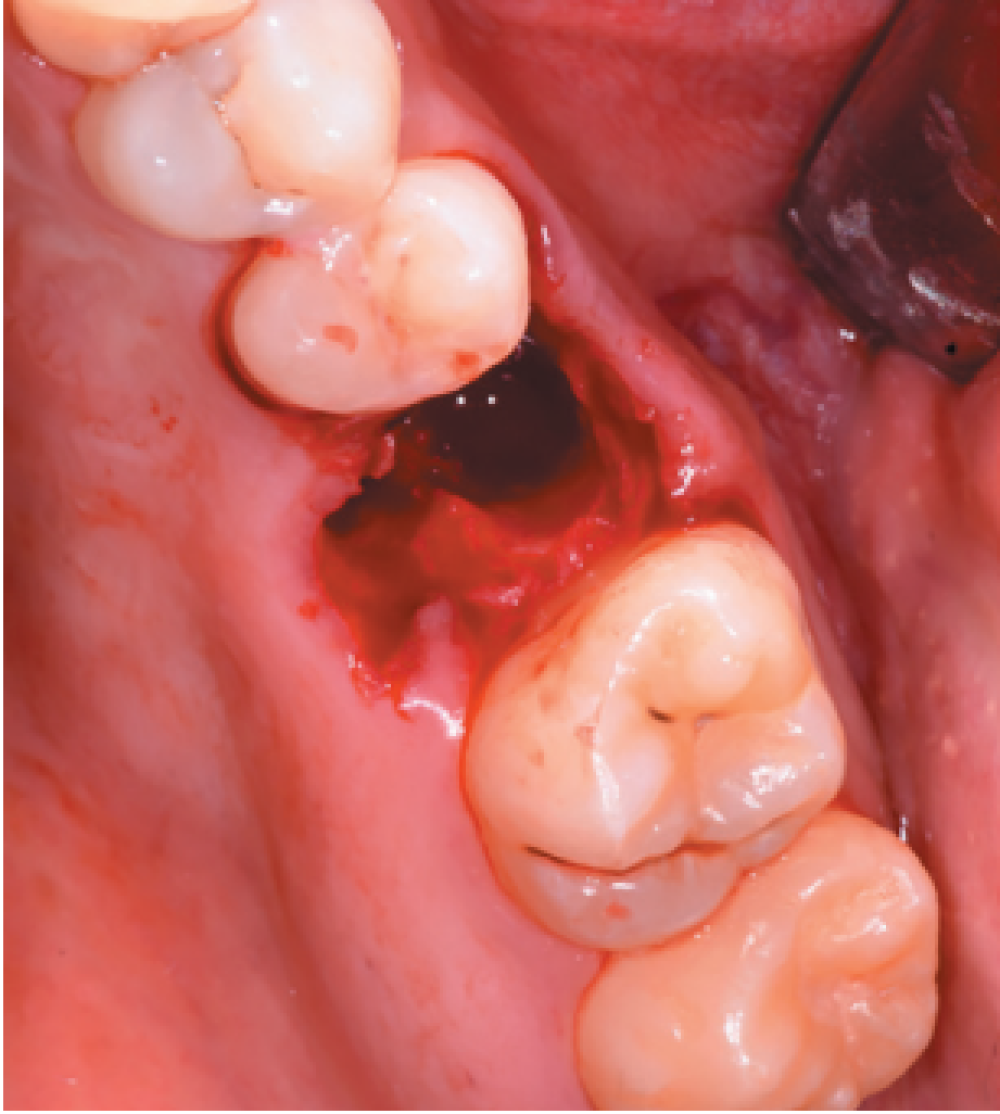
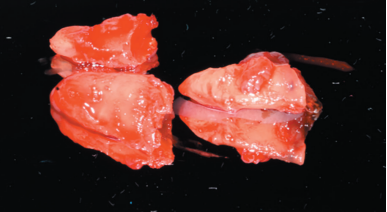
curett age of the apical process (Figure 6) was performed, leaving the alveolus of the 2.6 prepared to receive the autotransplant of the 2.8 (Figure 7).
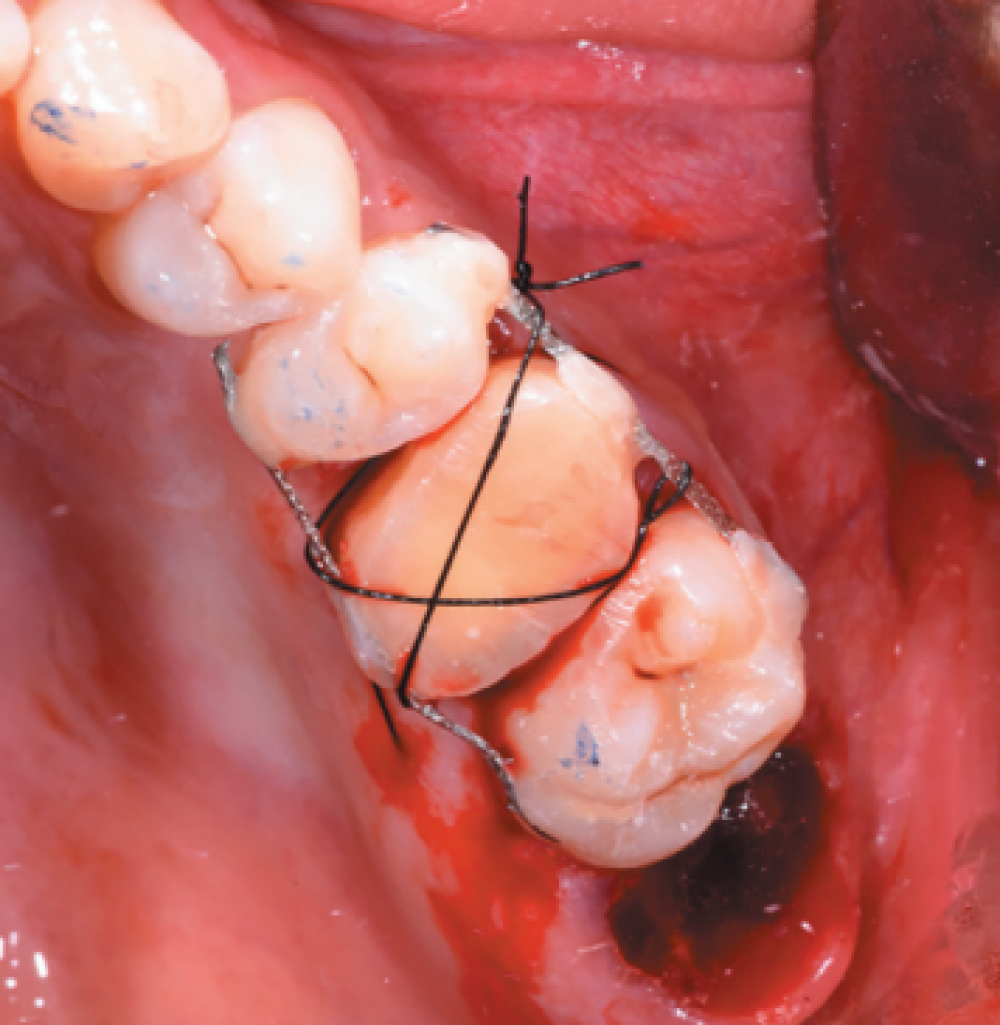
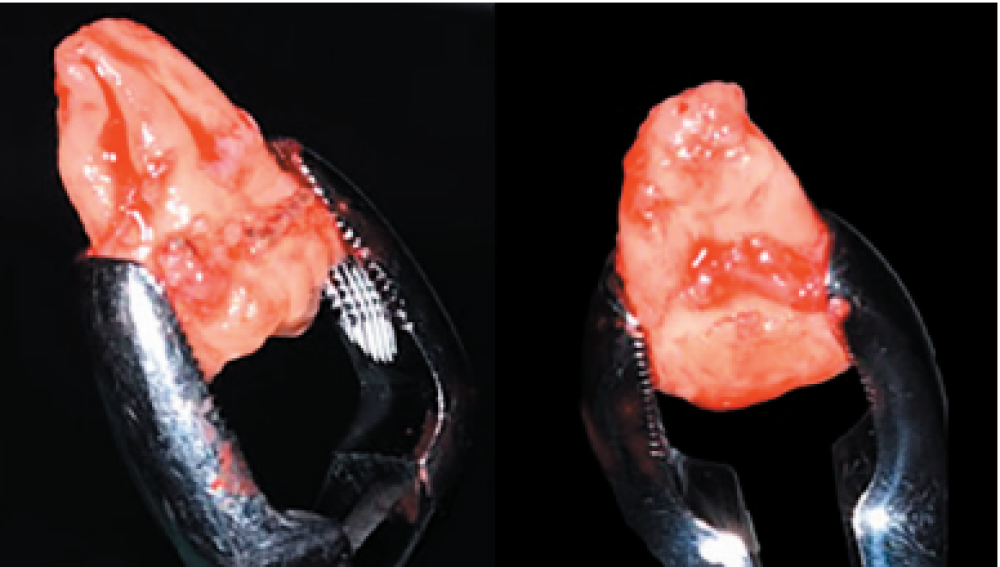
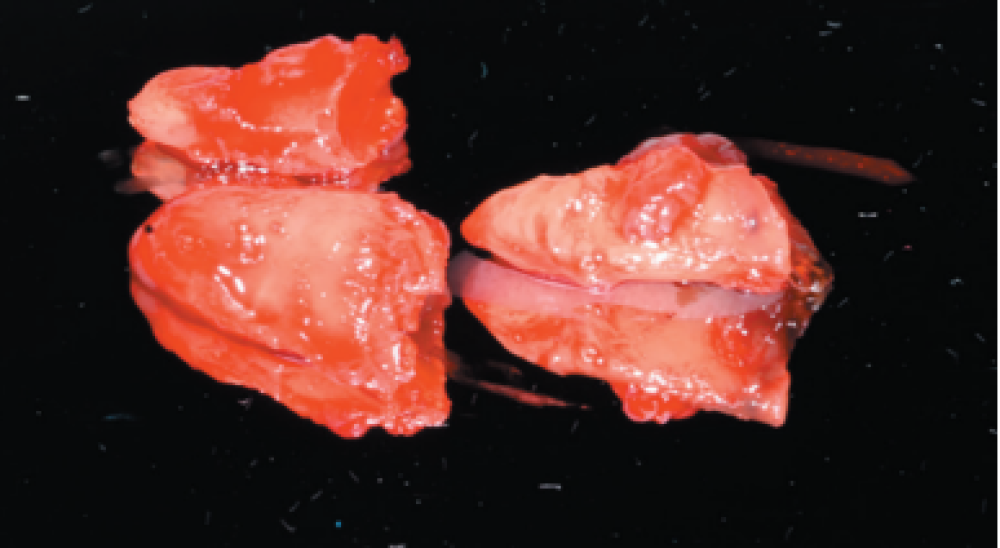
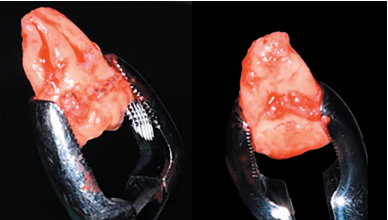
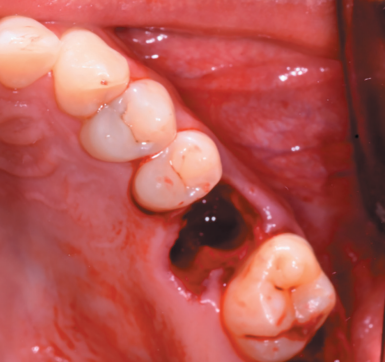
The 2.8 was then extracted with forceps (Figure 8), with minimal manipulati on of the periodontal ligament of the third molar, placing the upper third molar in the position of the upper fi rst molar (Figures 9 and 10).
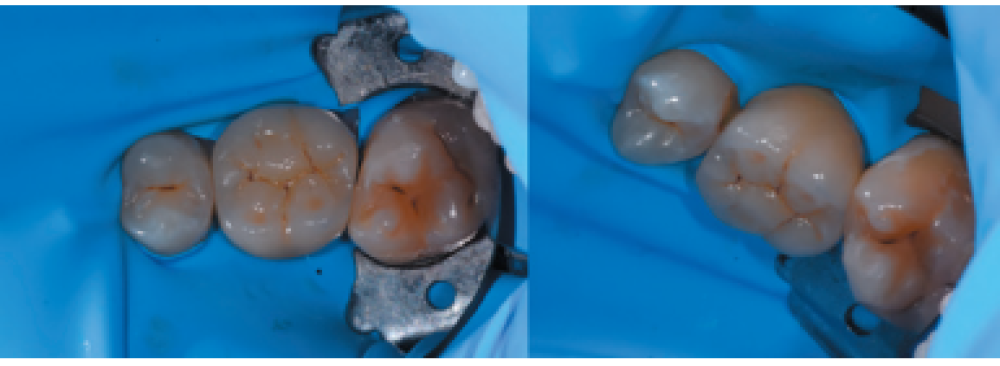
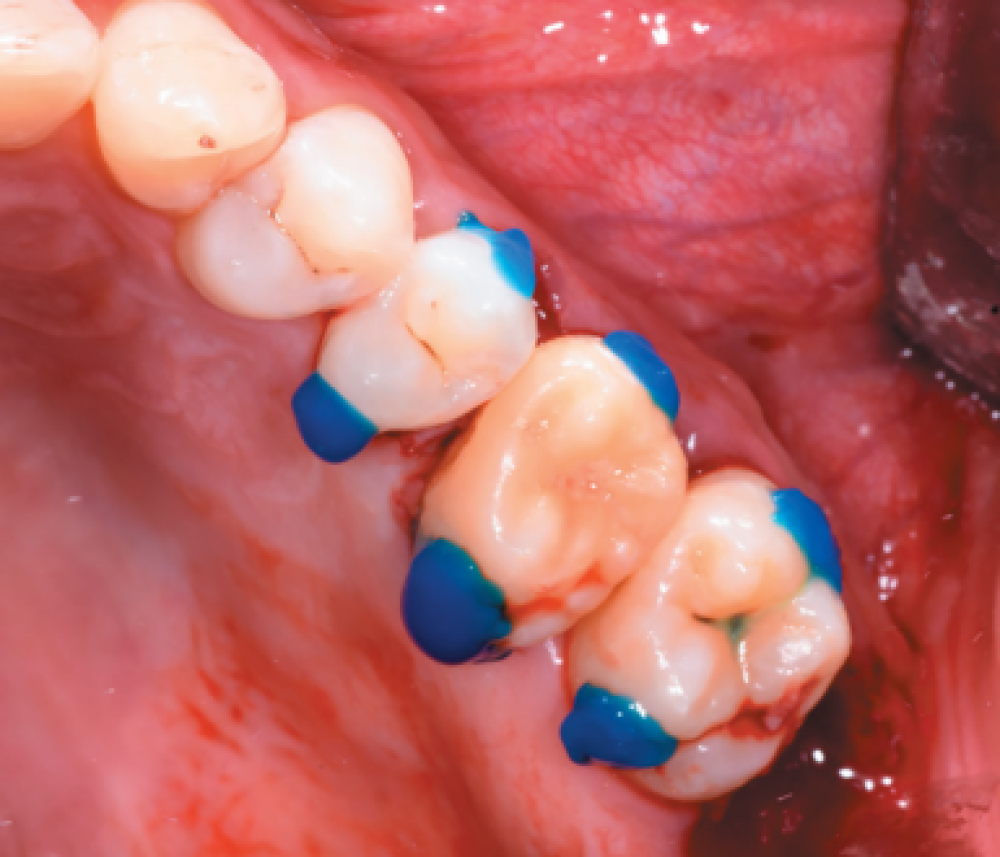
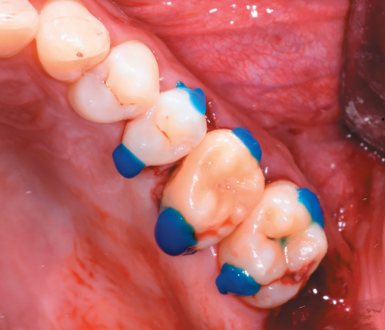
The 2.5, 2.6 and 2.7 teeth were then prepared by etching with orthophosphoric acid at 37% (3M Scotchbond UniversalTM, Minnesota, USA) for 20 seconds (Figure 11). After heavy washing of the etched surface with water, self-etch adhesive (3M Scotchbond UniversalTM, Minnesota, USA) was applied to fix the rigid wire with fluid composite resin (CharismaTM, Kulzer, Hanau, Germany) and conventional composite resin (G-aenialTM, GC, Leuven, Belgium) (Figure 12).
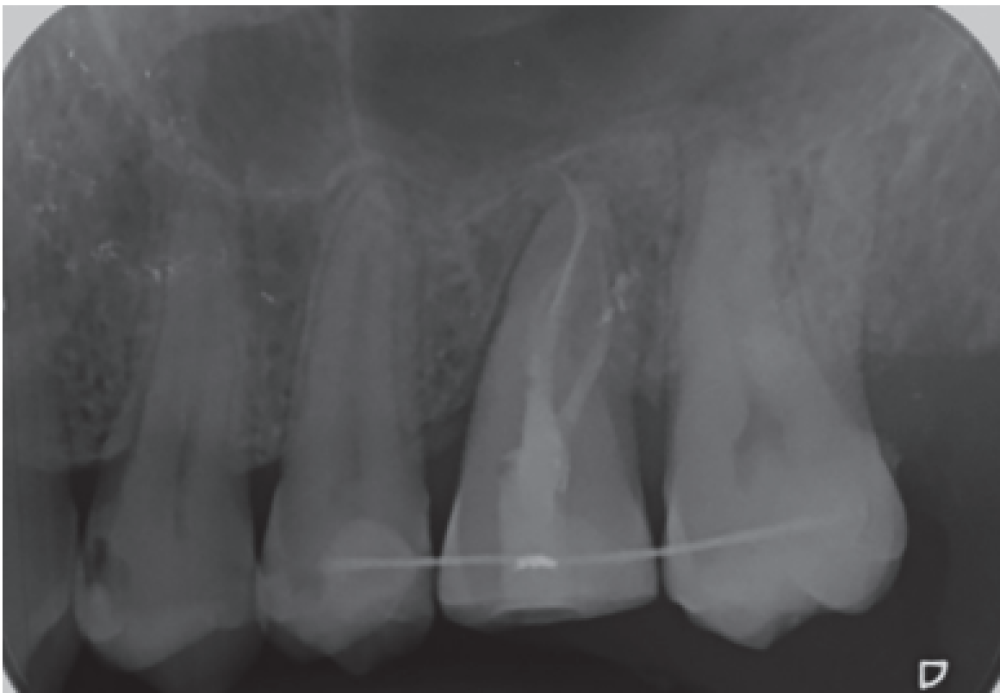
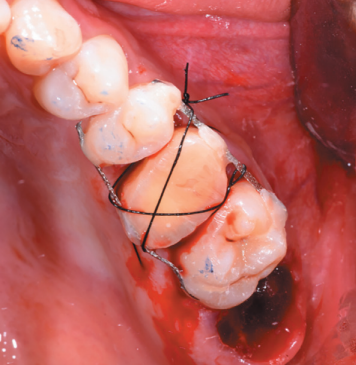
After reducing the occlusion, a cross stitch with monofilament suture (AragoTM, Barcelona, Spain) was applied around the transplanted tooth to increase its fixation (Figure 13), performing an intraoperative periapical radiograph with parallelism technique (Figure 14).
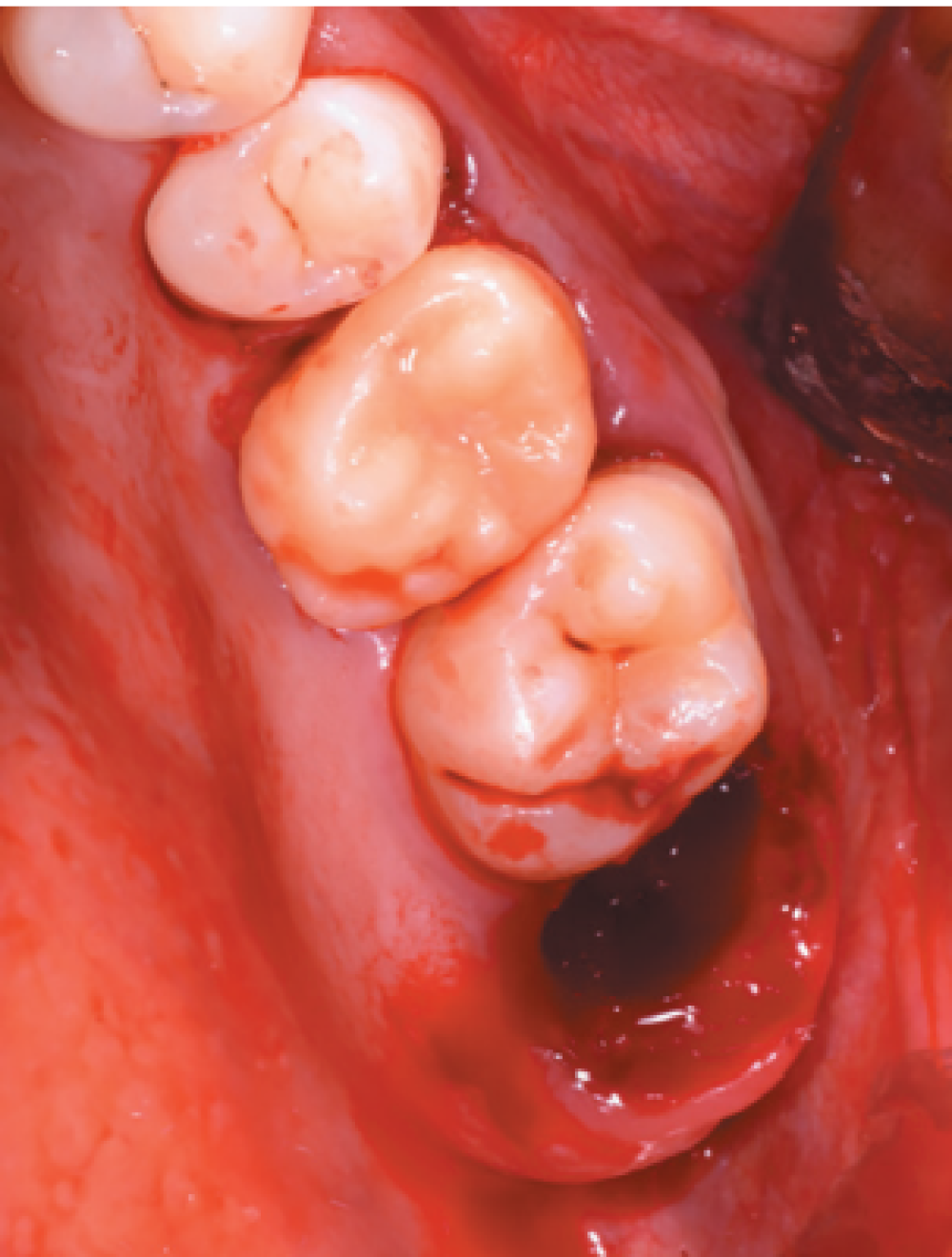
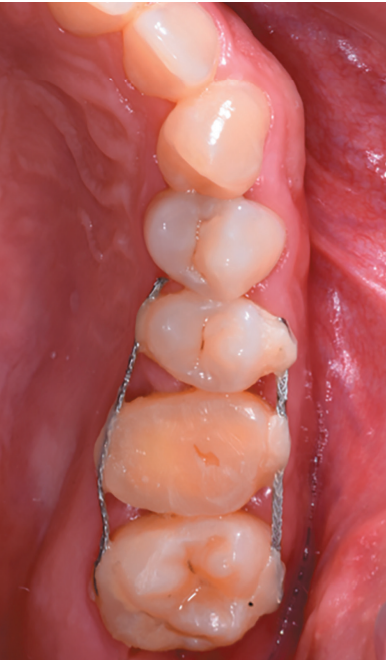
After ten days the suture was removed, where good soft tissue healing was observed (Figure 15). Three weeks after the postoperative period, treatment of the ducts was performed with a correct evolution (Figure 16).
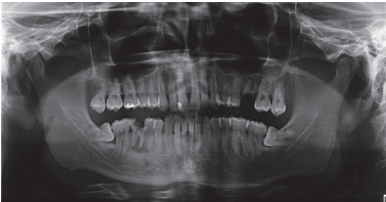
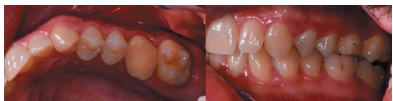
After 2 months, a new clinical review (Figure 17) and a radiograph was performed by a periapical radiograph (Figure 18), proceeding to remove the ferulization. After 3 months, another clinical review (Figure 19)
and a radiograph was performed by parallel periapical radiograph (Figure 20), where an adequate bone formation can be observed around the transplanted tooth.
After 5 months the autotransplant tooth was carved on its occlusal, vestibular, palatal and interproximal faces, then a heavy and fluid silicone double impression was taken in one step (Elite HDTM, Zhermack, Rovigo, Italy), and then ordered the laboratory a lithium disilicate inlay (Figure 21).
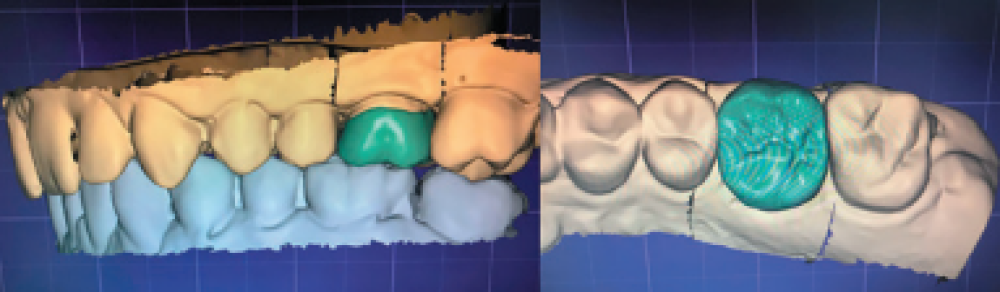
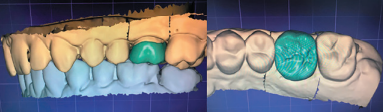
In the laboratory, the impression was casted and the upper and lower models scanned using the identical T710 MeditTM scanner for the computer inlay design and construction, using the Exocad PlovdivTM software (Figure 22).
The lithium disilicate inlay was milled, which was prepared at the clinic by etching with hydrofluoric acid and silane (UltradentTM, Madrid, Spain) (Figure 23).
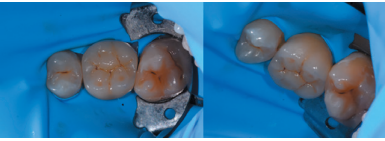
After that, the teeth 2.5, 2.6 and 2.7 were completely insulated by rubber dam, and tooth 2.6 was prepared with orthophosphoric acid and self-etching adhesive, and then cemented the inlay with dual polymerization resin cement (3M Relyx UnicemTM, Minnesota, USA). (Figure 24). After polymerizing for three seconds, the excess cement was removed, finished polymerizing and the rubber dam was removed to adjust the occlusion (Figure 25) and make a verification with a periapical radiograph (Figure 26).


2.8 transplanted in the alveolus of the 2.6.
withdrawal.
Although it is an effective therapeutic alternative, dental autotransplants are not currently a very popular treatment1,2, due to the development of dental implants3, although they represent the only treatment that allows a natural, functional and aesthetic rehabilitation4.
In this sense, autotransplants are economical procedures and one of the best dental replacement options when they are successful8,10,13. They are 87% cheaper compared to dental implants14, allowing in additi on, the placement of an implant if the autotransplant fails10, ensuring the maintenance of the alveolar bone due to physiological sti mulati on of the periodontal ligament5,15. However, the technique is very sensiti ve and the presence of a donor tooth is needed10.
The risk factors in performing autotransplants on teeth with closed apex are elderly pati ents, probing depths greater than 4 mm, previous duct treatment history, multi rooted teeth, donor teeth with caries and absence of vesti bular cortex16. In additi on, other factors are described that may infl uence the prognosis of these autotransplants, such as root anatomy, the degree of adaptati on of the donor tooth in the recipient bed (a greater degree of adaptati on is related to a greater percentage of healing and success)13,17, the durati on of the procedure (extra-alveolar ti me of the transplanted tooth), the experience of the surgeon (important to perform the extracti on of the donor tooth as atraumati cally as possible), the general health of the patient and the degree of oral hygiene, the existence or not of occlusal contacts during the healing period, and the timing and quality of treatment of transplanted tooth ducts8,18,19.
In this case, the treatment of ducts was performed aft er 3 weeks of the autotransplant, in accordance with other published studies6,20, where there are meta-analysis that conclude that conducti ng the ducts treatment two weeks aft er autotransplant reduces by half the probability of root resorpti ons11.
In the literature, most of the autotransplanted teeth are upper and lower third molars (73.9%), since they are usually non-functi onal teeth16. In this pati ent, advantage was taken of the presence of an erupted third molar, thus assuming a conservati ve therapeutic alternative for a young pati ent. Aft er the placement of the donor tooth in the recipient bed, the occlusion was reduced to avoid occlusal contacts and to allow periodontal healing after the autotransplant, also in accordance with the literature6.
Another of the fundamental aspects for the success of autotransplants is based on the type and duration of the ferulization, which are variable in the literature, coinciding in that ferulization should be used for a short period to achieve maximum physiologic benefits21. Authors such as Kokai et al.,20 believe that when the ferulization is maintained for more than 4-8 weeks, the risk of ankylosis is significantly increased, with other authors performing ferulization for only two weeks12. Therefore, in accordance with the literature, ferulization was maintained for 8 weeks in the case presented, in order to avoid the risk of ankylosis.
The published clinical studies evaluate patients clinically and radiographically, by periapical radiographs9,10,12,15,17,18 or by periapical and panoramic radiographs4,13,14. The periapical radiography shows the presence of radiolucent areas, external and internal root resorptions, ankylosis and the state of root development18, being fundamental in the evolution of this therapeutic modality. In the present clinical case, a radiolucent area around the tooth was radiographically visible, which was modified over time, to achieve a similar bone density of the bone in contact with the transplanted tooth, compared to the surrounding bone. Additionally, no apical lesions or root resorption were observed during the followup period.
In addition, a good clinical and radiographic result was obtained, after 5 months of follow-up, describing the patient a good masticatory function and the absence of adverse effects, which are described in the literature with a rate of 4%, highlighting among them the ankylosis and root resorption.
Clinical and radiographic follow-up is vital to determine the apical state of the autotransplant, so one of the limitations of this technique would be to have uncooperative patients, who are not aware of the need of an adequate maintenance programme and revisions2. Authors such as Tsukiboshi et al.,7 suggest that, in the case of autotransplants that have healed correctly, periodic revisions should be made with the frequency of the rest of the teeth.

autotransplant, coinciding with the duct treatment.
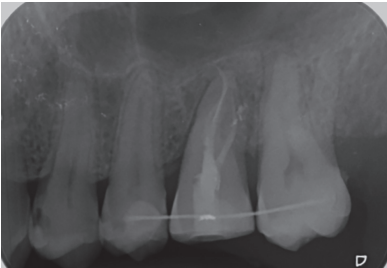
autotransplant.
autotransplant.


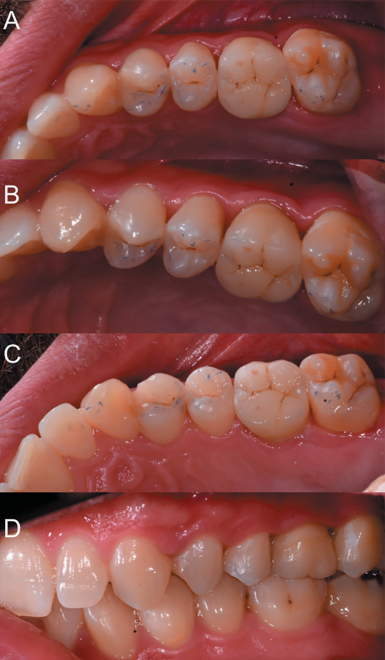
palatine (C), occlusion (D).
autotransplant.
Dental autotransplants are a therapeutic alternative with high success rates, which can replace dental implants in well selected cases, favouring the acceptance rate by the patient, being an autologous material, which favours the development of the alveolar bone, and which does not prevent, in addition, the placement of implants if the autotransplant fails.
Autotransplants and dental implants are two surgical techniques with identical objectives. While the former has more limited indications, requiring a more sensitive technique, with a lower economic cost for the patient and a simpler restoration for the professional, dental implants lack eruptive and movement capacity, not being recommended in growing patients.
The autotransplants undergo micromovements and achieve occlusal harmony in relation to the adjacent teeth, offering better aesthetic results and a better emergence profile.
Machado LA, Do Nascimento RR, Ferreira DM, Mattos CT, Vilella OV. Long-term prognosis of tooth autotransplantation: a systematic review and meta-analysis. Int
Martin K, Nathwani S, Bunyan R.
Autotransplantation of teeth: an evidencebased approach. Br Dent J 2018; 224 (11): 861-4.
Abela S, Murtadha L, Bister D, Andiappan M, Kwok J. Survival probability of dental autotransplantation of 366 teeth over
34 years within a hospital setting in the United Kingdom. Eur J Orthod 2019;41 (5): 551-6.
Strbac GD, Giannis K, Mittlbock M, Furst G, Zechner W, Stavropoulos A et al. Survival rate of autotransplanted teeth after 5 years-A retrospective study. J Craniomaxillofac Surg 2017; 45 (8): 1143-9.
Park JH, Tai K, Hayashi D. Tooth
autotransplantation as a treatment option: a review. J Clin Pediatr Dent 2010; 35 (2): 129-35.
Dioguardi M, Quarta C, Sovereto D y cols. Autotransplantation of the third molar: a therapeutic alternative to the rehabilitation of a missing tooth: a scoping review. Bioengineering (Basel) 2021; 8 (9): 120.
Tsukiboshi M. Autotransplantation of
teeth: requirements for predictable
success. Dent Traumatol 2002; 18 (4):
157-80
Almpani K, Papageorgiou SN,
Papadopoulos MA. Autotransplantation of teeth in humans: a systematic review and meta-analysis. Clin Oral Investig 2015; 19 (6): 1157-79
Tsukiboshi M, Yamauchi N, Tsukiboshi Y.Long-term outcomes of autotransplantation of teeth: a case series. Dent Traumatol 2019; 35 (6): 358-67.
Nagori SA, Bhutia O, Roychoudhury
A, Pandey RM. Immediate
autotransplantation of third molars: an experience of 57 cases. Oral Surg Oral Med Oral Pathol Oral Radiol 2014; 118 (4): 400-7
Boschini L, Plotino G, Melillo M, Staffoli S, Grande NM. Endodontic management of an autotransplanted mandibular third molar. A simplified approach. J Am Dent Assoc 2020; 151 (3): 197-202.
Boschini L, Melillo M, Berton F. Long term survival of mature autotransplanted teeth: a retrospective single center analysis. J Dent 2020; 98: 103371.
Erdem NF, Gumuser Z. Retrospective
evaluation of immediate impacted
third molars autotransplantation after
extractions of mandibular first and/or
second molars with chronic periapical
lesions. J Oral Maxillofac Surg 2021; 79 (1): 37-48.
Ong DCV, Dance GM. Posterior tooth
autotransplantation: a case series. Aust Dent J 2021; 66 (1): 85-95.
Murtadha L, Kwok J. Do autotransplanted teeth require elective root canal therapy?
A long term follow-up case series. J Oral Maxillofac Surg 2017; 75 (9): 1817-26.
Yoshino K, Ishizuka Y, Sugihara N y
cols. Risk factors affecting third molar
autotransplantation during 5 and 10
years: a retrospective clinical survey. Bull Tokyo Dent Coll 2014; 55 (2): 111-22.
Ashurko I, Vlasova I, Yaremchuk P,
Bystrova O. Autotransplantation of teeth as an alternative to dental implantation. BMJ Case Rep 2020; 13 (6): e234889.
De Freitas Coutinho NB, Nunes FC,
Gagno Intra JB y cols. Success, survival rate and soft tissues esthetic or tooth autotransplantation. J Endod 2021; 47 (3): 391-6.
Xia JJ, Ge ZY, Fu XH, Zhang YZ.
Autotransplantation of third molars with completely formed roots to replace compromised molars with the computeraided rapid prototyping. J Esthet Restor Dent 2020; 32 (3): 265-71.
Kokai S, Kanno Z, Kolke S y
cols. Retrospective study of 100
autotransplanted teet with complete root formation and subsequent orthodontic treatment. Am J Orthod Dentofacial Orthop 2015; 148: 982-9.
Armstrong L, O´Reilly C, Ahmed B.
Autotransplantation of third molars:
a literature review and preliminary
protocols. Br Dent J 2020; 228 (4): 247- 51.

Sánchez-Labrador Martínez
de Morentin, Luis
Professor of Master in Surgery Buccal and Implantology Universidad Complutense de Madrid (UCM)
Domínguez Marsal, Begoña
Advanced Endodontics Master’s Degree Universidad Europea de Madrid (UEM), Lecturer degree UEM.
Cortés-Bretón Brinkmann,
Jorge
Associate Professor UCM.
Barona-Dorado, Cristina
Contracted Professor UCM.
Martínez-González, José
María
Maxillofacial surgery Professor
UCM.