Biblographic review
Published in spanish Científica Dental Vol. 20. Nº 2. 2023
Influence of non-alternating unilateral mastication in maxillofacial development and early treatment
Introduction: Non-alternating unilateral chewing is a harmful habit consisting of exclusively or predominantly chewing on one of the two sides of the dentition that, maintained over time during growth, causes an asymmetric development of the craniofacial structure affecting bone, muscle, joint and dental structures.
Objective: To describe how unilateral chewing influences maxillofacial growth and occlusion, as well as the early approach to avoid the consequences of this habit.
Material and method: A bibliographic search was made in the EBSCO-Dentistry Oral Science Source meta-search engine and in PubMed, selecting full-text articles in English and Spanish related to the subject, from which 45 were extracted to make this review.
Results: Non-alternating unilateral mastication generates the mandibular ramus of the non-masticatory side to undergo a greater growth because the condyle of this side only performs translational movements with an enormous growth stimulus. In addition, the greater load in the condyle of the chewing side generates anatomical changes, the neck being thickened and the head area increased. These changes at mandibular level produce unilateral posterior crossbite on the mastication side with a class II subdivision.
Conclusions: The hyperfunction of the mastication muscles and the vertical mandibular movement on the chewing side, as well as the eminently translational trajectory on the steady swinging side, generates asymmetric growth of the jaw and TMJ, deviation of chin and inferior dental midline to the working side, unilateral posterior crossbite and class II subdivision on the mastication side, among other alterations. Therapeutics in early stages consists of function rehabilitation, applying composite tracks on the cross side and maxilla expansion.
The growth and development of the craniofacial structure is the result of the interaction between genetic and environmental factors where there is an increase in size, remodelling and displacement of structures1. They are morphogenic processes aimed at a state of functional and structural equilibrium between all the regional parts of the hard and soft tissue in growth and development. To achieve a physiological occlusion, the jaw will assume a greater growth in length than the maxilla1,2. The bones grow by the apposition of new bone tissue on one side of the cortical and resorption in the opposite area. This compound process is called drift and creates a direct growth movement of any given bone area.
The genetic and functional determinants of bone growth lie in the set of soft tissues (muscles, tongue, lips, cheeks, tonsils, adenoids…) that activate, deactivate, accelerate and delay the histogenic actions of osteogenic connective tissues1. During this growth, physiological habits (speech, normal swallowing and chewing) are stimuli for the growth of these structures. However, there are a number of harmful habits such as digital suction, onychophagia, oral breathing or lingual interposition that can interfere in maxilla and mandibular development and be part of the aetiology of malocclusions3.
According to Proffit’s theory of equilibrium, intense and intermittent functional forces are resisted by physiology, while light and continuous postural forces lead to adaptive mechanisms that produce biological remodelling4. These parafunctional oral habits of the stomatognathic system modify the position of the teeth and the relationship between them, as well as normal growth and function of the orofacial musculature, producing an imbalance between internal and external muscle forces5,6. Early diagnosis of abnormal habits is crucial for the prevention or early correction of malocclusions that may develop6.
A basic postulate of functional cranial analysis is that the structure of the head and neck is organized operatively in terms of function: digestion, vision, olfactory sense, speech, etc.7. According to the Moss functional matrices hypothesis, each of the functions is performed by a functional cranial set. These components consist of two parts: a functional matrix that performs the function and a skeletal unit whose biomechanical role is to protect and/or support its specific functional matrix. Skeletal units are those formed by bone, cartilage or tendon tissues. Functional matrices include muscles, glands, nerves, vessels, fat, and teeth8.
Unilateral chewing occurs when chewing is performed constantly or predominantly by one of the two sides of dentition. Both the jaw and the condyle modify their shape and size if the habit is maintained during development9,10.
The objective of this bibliographical review is to elucidate the changes that can be produced by non-alternating unilateral mastication during development in the different structures of the craniofacial structure, as well as determine the causes for which this habit develops and describe the early approach during growth to prevent these alterations.
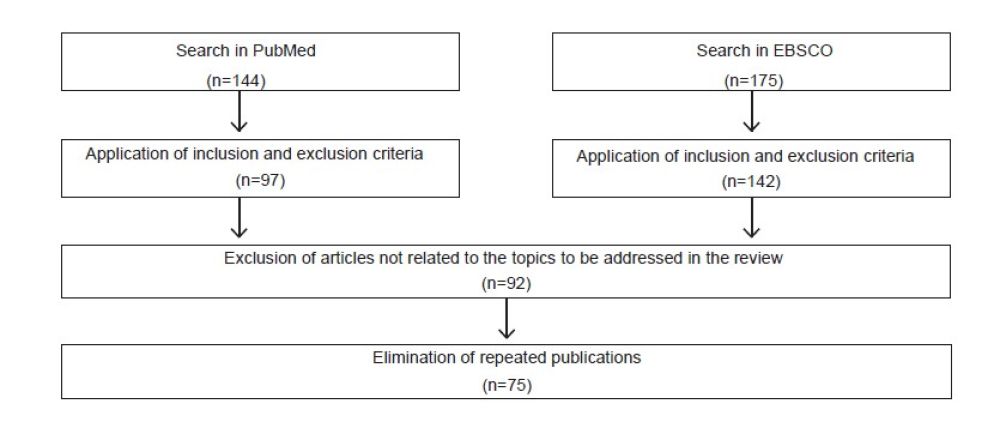
To perform this bibliographical review, two searches were carried out. The first was carried out in the Discovery Service (EBSCO) metasearch engine, specifically in the section: Dentistry & Oral Science Source. The boolean operators “OR” and “AND” were used and the following search terms were introduced: “unilateral chewing”, “mandibular asymmetry”, “unilateral posterior crossbite”, “treatment” and “causes”. 175 articles were found. The search was then filtered with the following inclusion and exclusion criteria:
Inclusion criteria:
• Articles in Spanish or English.
• Full text.
• Academic publications.
Exclusions criteria:
• Articles in a language other than Spanish or English.
The result was reduced to 142 articles.
The second search was carried out in the PubMed search
engine using the same boolean operators and the same terms as in the first search. A result of 144 articles was obtained. The search was then filtered using the same inclusion and exclusion criteria as above. The result was reduced to 97 articles. Given the low volume of publications, all articles were considered without publication date limitation.
Then, we proceeded to reading the titles in both information resources discarding those articles which were not in line with the topics to be addressed in this bibliographical review.
Among the publications obtained from Discovery Service (EBSCO) and PubMed, 92 articles were selected. Of these 92 publications, 17 were repeated. This article selecting process relevant to this study is presented in the following flowchart (Figure 1):
We proceeded to read the 75 articles and we discarded 30 in which no outstanding information was found for the development of the work. 45 were used to make this bibliographical review. In addition, two reference books, three web pages publications and six articles with relevant information from other sources were included.
All growth changes in size, shape, spatial position and maintenance of all skeletal units are always secondary to the primary temporal changes in their specific functional matrices. Noticeable changes are perceived in the jaw when the mastication temporalis, masseter and internal pterygoid muscles increase their function and cross-sectional area1,8.
When chewing is performed with predominantly vertical movements, as in the case of non-alternating unilateral mastication, the dominant muscles are the masseter, external pterygoid and anterior fascicle of the temporalis, generating a hinge movement on the masticatory side. The articular eminence of the temporal is accentuated because there is no condylar translation11.
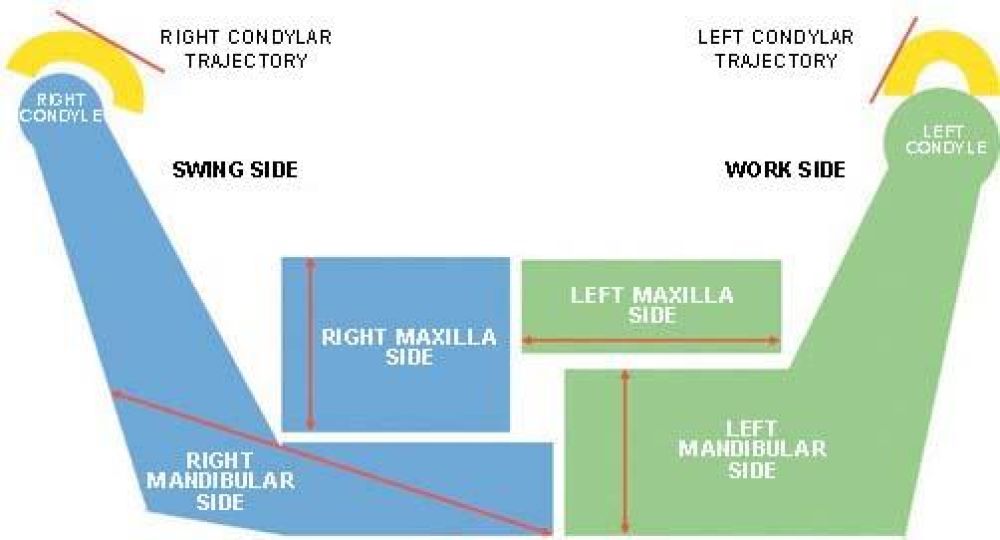
The neck and the mandibular condylar show traces of the reaction against major masticatory loads, especially of asymmetric type as in this type of chewing. To face these loads, the neck of the condyle thickens and the mandibular condylar area increases significantly1. The condyle on the chewing side performs only a rotational movement, so it lacks a growth response. In addition, it suffers an excessive burden resulting in anatomical and structural changes in the TMJ. On the opposite side, the condyle performs only translational movement, causing a growth response with elongation of the neck and mandibular ramus and remodelling of the condyle-disc structure2.
According to Planas’ “Anteroposterior and Transverse Growth Law”, the anteroposterior excitation of the TMJ of the swinging side produces as response the growth in length of the mandibular ramus of this side. However, on the working side the functional occlusal rub produces a mandibular thickening and expansion, thus producing a mandibular asymmetry12.
To analyse this condition, a combined clinical analysis is necessary with front and side photographs, lateral and anteroposterior cephalogram, oblique mandibular X-rays at 45° and panoramic X-rays. The clinical analysis includes the electromyographic study, observing the location of the bolus in the oral cavity and the mandibular movement in the closing phase of the mastication13,14.
In addition, when analysing the vertical dimension in these patients, it will be observed that, during the right to left lateral excursions, the vertical dimension is smaller on the chewing side. These measurements can be recorded in the front plane when performing the lateralities, the “Planas’ functional masticatory angle”11. being defined.
There are several types of foods that have been used as a test to determine the preferred chewing side in patients. In most studies chewing gum is used, but carrots and almonds have also been used. Other products such as silicone tablets can be used. The size, hardness and texture of the bolus influences the masticatory cycle and its muscle activity15.
In addition, other evaluations can be performed such as video recording, kinesiography or electromyography16.
Non-alternating unilateral mastication can occur for several reasons: mediation of the Central Nervous System and relationship with other laterality preferences such as being right or left-handed, peripheral factors such as avoiding one side because it produces pain or preference on one side for greater chewing efficiency. It may also be due to dental factors, size and type of ingested food, and the number and duration of chewing cycles until swallowing17.
According to Larato, the teeth of the side that does not chew accumulate more dental calculus and plaque in their crowns and roots and as a consequence produce bone loss. This side presents a higher height of the canines, resulting in interference instead of acting as a canine guide. As a consequence, a worse occlusion adjustment occurs, making the patient chew with the easier half arch18,19.
Patients with facial asymmetries not only present this deformity on the outer surface, but also in the internal structure as to the shape of the dental arch and the oral or lingual pressure, when comparing the two half arches. A deviation of the lower midline can be observed along with the chin toward the mastication side with a displacement of the lower interincisive point, being common the appearance of a crossbite. A class II subdivision occurs on the chewing side due to mandibular displacement toward that side2,20.
As it is known, posterior crossbite is a transversal malocclusion in which the palatal cusps of one or several superior teeth do not occlude in the central fossa of their antagonists and it is the vestibular cusps that do so. It occurs on the side where mastication predominates, where the mandibular ramus is shorter13,21. On the crossbite side -the side used to chew- a hypertrophy of the masseter occurs due to the excessive use. These patients appear to have a dolichofacial pattern in half of their face on -the side without chewing-, while in the other half of the face they appear to have a brachyfacial pattern22.
It has been suggested that an altered morphological relationship between the upper and lower arch is associated with differences in the condylar fossa relationship between the right and left side23. Any association between a temporomandibular disorder and a malocclusion, such as posterior crossbite, indicates the need for early orthodontic treatment to avoid future problems with joints and masticatory muscles24.
It is very important to make a good anamnesis to know the patient’s history, looking for possible factors that trigger and favour this type of habit4. Elimination of the habit and early treatment are necessary, since malocclusions with a skeletal component tend to worsen over time. The prognosis of malocclusions is aggravated if the start of treatment is delayed or if inappropriate treatment is applied: the imbalance between form and function increases22.
Asymmetric malocclusions are often complicated to correct, especially when there is an underlying skeletal component. The optimal treatment for this condition will depend on its severity and the age of the patient22,25,26. According to Proffit, when the patient is growing it is possible to try to control and modify this asymmetric growth26. A first phase of orthopaedic treatment is allowed to avoid orthognathic surgery when growth ends. In adults, however, skeletal asymmetries are usually treated by combining orthognathic surgery and orthodontics25.
In addition to correcting the crossbite, the professional should also concentrate on rehabilitating the function. If the correction were to focus solely on the form, uncrossing the bite, and the patient continues to chew on the corrected side, the malocclusion would tend to recur2. To stimulate the function, the patient must chew gum on the side that does not have the crossbite to stabilize the correction. This will progressively improve the masticatory function and mandibular rest position22.
According to Plans’ minimum vertical dimension law, the side with the masticatory preference will have the lowest canine guide, minor posterior disocclusion and will present a minor Masticatory Functional Angle. Therefore, it will be necessary to perform selective reduction and apply composite tracks2,12. These tracks are composite resin aggregates that act as inclined planes to position the jaw and achieve a different intermaxillary relationship. The technique tries to add composite to the canine on the cross side to increase the canine guide on that side and make chewing difficult. The tracks can also be built on the occlusal faces of molars from lingual to palatine on the side of the crossbite. They are a very good option, since they do not need the patient to be collaborative and they remain active 24 hours a day and the 7 days of the week2,27. They are constructed in such a way that, when performing lateral movements, the Planas’ Functional Masticatory Angle is smaller on the non-crossed side to functionalize it. If necessary, selective reductions could be made so that the vertical dimension remains smaller on the non-crossed side. In this way we try to change the functional side12.
If selective reductions alone are not effective, an upper removable expansion plate can be used at an early age to expand the maxilla, thus reducing the risk of lengthening the posterior crossbite28,29. According to Del Pinal et al., the most used device for slow expansion is the Quad-Helix. It performs a symmetrical expansion of the arch and an increase of its vertical dimension through reciprocal forces on the teeth. In 75% of the cases it produces a discreet opening of the palatal suture. In late ages such as 10 years old, it produces effects only at the dentoalveolar level27.
There are several causes that can make an individual to establish a non-alternating unilateral chewing as a usual masticatory pattern in their day to day. When analysing with visual control and T-Scan the chewing of 100 people, 50 with unilateral non-alternating right mastication and 50 with unilateral non-alternating left mastication, it was concluded that the participants preferred one side or another depending on the contact area between the teeth, being greater on the preference side. Other studies that use wax for the analysis of this condition report this. Haralur et al. state that wax presents poor dimensional stability, so it is not possible to analyse small occlusal contacts. The T-Scan sensors are 98 nanometres thick, while the wax is 0.5 to 0.75 mm30.
Non-alternating unilateral mastication can also be influenced by other parameters such as laterality contacts, occlusion, cuspidal shape, posterior teeth absence, interference on the working side and the size and consistency of the ingested food. In addition, oral sensorimotor systems and pulp nociception, periodontal and articular tissue are also related to mastication behaviour31-33. Pond et al. state that these occlusal factors are influential when the mastication pattern is developing in the child, but when this pattern is established, only painful stimulation can change it34.
In their study, Nissan et al. compared the preference of the mastication side with the preference in the use of the feet, hands, eyes and ears to see if it is another hemispheric lateralization such as these last conditions, this relationship being positive31. However, Wilding et al. state in their work that some studies reject this and that, while the preference for using mostly one of the hands, eyes or ears is centrally controlled, the preference for one mastication side is determined by peripheral factors such as masticatory efficiency or comfort35. The first impulse to bite and chew a food is a voluntary act, but subsequently becomes an involuntary act mediated by central and peripheral neural mechanisms33.
According to the Moss’ functional matrix hypothesis, the growth of a bone and its changing position in space are related to the growth of the muscle that is inserted into it36. This is reinforced by Mew, who states that changes in mandibular growth are effected by the cells of this bone, which act in response to positional information they receive from the tissues around the jaw.
It has been shown that the formation, growth, size, shape, spatial position and maintenance of the mandibular angular process are always secondary to the functional demands of the masseter and medial pterygoid muscles9,28,29. In the analysis of a corpse performed by Rogers, it was observed that the right masseter was one fifth the size of the well developed left masseter. The left temporal was medium in size, while the right was completely absent. In addition, the pterygoid muscles on the right side had a cross-sectional area of about one-quarter of the left cross-sectional area. When studying the skull, he observed the complete loss of the alveolar crest on the side with well-developed muscles (left) compared to the very sharp alveolar crest on the atrophied side. This led him to conclude that the individual predominantly performed the mastication on the left side37.
The areas of muscle insertion in the mandibular ramus play an important role in the local remodelling and in the cortical displacement that accompanies the mandibular displacement downward and forward. If the masticatory activity of the muscles is asymmetric, the remodelling process will be altered causing a structural change. The strength of the masseter on the mastication side is transmitted to the jaw, which develops a greater trabecular bone on this side due to the higher mechanical requirement11. In experimental studies performed by Legrell, a shorter branch on the mastication side is observed with a compensation in bone growth at the mandibular base level and the goniac region38,39.
Augusto et al., when analysing a skull whose mastication was predominant on the left side, observed several consequences in its development. On the mastication side, the jaw was anteroposterior shorter, higher and with more volume and the upper maxilla wider transversely and anteroposterior. On the opposite mastication side, in anteroposterior direction, the jaw was longer and the maxilla was shorter and less developed (Figure 2)40.
The factor that determines the size of the dental arches are the facial muscles, the crowding or the space between the teeth. The bones have a secondary role41.
Regarding the temporomandibular disorders, there is no clear consensus on the association between non-alternating unilateral mastication and temporomandibular disorders. Some epidemiological studies have shown that people with non-alternating unilateral mastication have a higher probability of developing temporomandibular disorders. This habit excessively loads the TMJ on the preferred mastication side with respect to the contralateral side, producing anatomical and structural changes in the cartilage, the glenoid cavity and the condyle. The significant statistical relationship between the mastication side and temporomandibular disorder symptoms is inherent42,43. However, in a study performed with a CBCT scan to compare the condylar position between patients with habit and without habit, no differences were reported between them42.
Santana-Mora et al. confirm that chronic unilateral temporomandibular disorders mainly affect the usual mastication side, with a higher condylar path and flatter anterior lateral guide angles. This allows us to conclude the hypothesis that the preferred mastication side may be a factor that leads to the development of temporomandibular disorders and a remodelling of the masticatory apparatus44.
On the other hand, a study performed at the Dentistry Faculty of the University of Chile that analysed different types of temporomandibular disorders concluded that there were no significant differences in the presence of temporomandibular pathology between unilateral mastication patients and alternating unilateral masticating patients14.
In a study evaluating the bone morphology of the TMJ in patients with alternating and non-alternating unilateral mastication, significant differences were observed in the joint space, joint fossa depth, the width of the condylar neck and the inclination of the articular eminence -which is more pronounced- among the opposite TMJ, increasing the potential risk of developing a temporomandibular disorder. An asymmetry of the condylar trajectory is produced as an adaptive mechanism caused by the predominant use of a side45,46.
The relationship between the type of mastication and the presence of temporomandibular disorders is not clear, despite a high tendency of joint pathology in unilateral mastication patients14.
Regarding mandibular asymmetry and unilateral posterior crossbite that generates this habit, it has been concluded that patients with this transversal relationship present an alteration in the glenoid-disc-condyle fossa relationship also with an asymmetric skeletal growth. With an increase in the thickness of the cartilage of the contralateral side and a decrease in the mastication side. In addition, they frequently show an anterior disc displacement in the TMJ of the deviated side due to the constant tension and stress on the back of the disc23,47,78. Pullinger et al. confirmed that there is an association between unilateral posterior crossbite and some signs and symptoms of temporomandibular disorder such as joint pain, clicks, muscle tension, or headaches49.
Regarding the treatment of this condition, Petrén et al. confirm that the treatment of choice for the correction of a posterior crossbite in patients with primary dentition is the selective reduction of canines50. Facal also proposes selective reduction as the main option, decreasing the height of the canines of the non-chewing side below the height of the contralateral canines, thus performing a hypercorrection18. However, Planas proposes the composite tracks as the main treatment and, if necessary, perform a selective reduction of the canines12.
De Boer and Steenks indicate in their study that selective reduction of cusps of temporary teeth can intercept the growth and development of the masticatory system of patients. Reduction can be an option only if the difference of maxillary and mandibular width is greater than 3 mm in the canine region51. Malandris and Mahoney claim that selective reduction changes the chewing pattern, achieving more symmetrical movements and bilateral chewing52. Facal proposes to add crossed elastics in the second temporary molars and in the first permanent molars, if the patient had them, to increase the vertical dimension in case the composite tracks and reduction were not enough2.
Brin et al. confirm that the best way to treat a posterior crossbite in a mixed dentition is with slow expansion, since some degree of skeletal influence is expected at this age53. The most used device for this expansion is the Quad-Helix. Petrén et al. corroborate that this device is the best for the malocclusion treatment54. Quad-Helix can produce an expansion in the median palatine suture in 75% of cases along with orthodontic movements and dentoalveolar inclination. From 10 years old only acts at dentoalveolar level27.
One of the concerns of orthodontists is whether, by correcting the unilateral posterior crossbite, a change in the position of the condyle in the TMJ could occur, thus reducing the adaptive capacity of some patients. Therefore, the professional should consider whether the non-surgical correction of this malocclusion can have an impact on the state of the TMJ or whether it can lead to pain or discomfort25. However, several studies indicate that all symptoms of temporomandibular disorders that may exist, such as joint sounds, headaches, muscle pain or weakness associated with this condition, disappear after orthodontic correction27.
The non-alternating unilateral mastication habit generates a series of changes at muscle, bone and joint structures level of the TMJ, generating an asymmetric mandibular growth. This mandibular asymmetry generates a posterior crossbite on the chewing side in most cases.
This habit is determined mainly by peripheral factors such as occlusion, comfort in chewing, the contact area between the teeth, interference in lateralities, etc.
The increase in function and size of the mastication muscles on the preferred side will lead to changes in the TMJ and the jaw will be anteroposterior shorter, higher and bulkier.
At the TMJ level, alterations appear such as anterior disc displacement, lower disc thickness, more inclined articular eminence and thickened condyle. The association between non-alternating unilateral chewing, posterior crossbite and temporomandibular disorders is unclear.
The treatment of choice for the correction of non-alternating unilateral mastication with posterior crossbite during growth is the application of composite tracks in the cross-side and selective canine reduction in the non-crossed canine, if necessary, looking for the minimum vertical dimension, and therefore, mastication on this side. When it is not possible to correct it with tracks and reduction, maxillary expansion will be chosen.
Enlow DH. Maxillofacial Growth. 3Rd ed. Mexico City Nueva Editorial Interamericana; 1992.
Román Jiménez M. El problema transversal. Tratamiento precoz de la mordida cruzada desde los 4 años. Alternativa a la aparatología ortodóncica [Internet]. 2021 [Consulted 30 Oct 2022] Available at: https://manuelroman.com/ el-problema-transversal-tratamiento- precoz-de-la-mordida-cruzada-desde- los-4-anos-alternativa-a-la-
Rodríguez-Olivos LHG, Chacón- Uscamaita PR, Quinto-Argote AG, Pumahualcca G, Pérez-Vargas LF. Deleterious oral habits related to vertical, transverse and sagittal dental malocclusion in pediatric patients. BMC Oral Health 2022;22(1): 88-94.
Muñoz Ruiz J, Kahn S, Ruiz MM y cols. Orthotropics: un sueño hecho realidad. Rev Esp Ortod. 2016;46:108-21.
Ojeda Léonard C, Espinoza Rojo A, Biotti Picand J. Relación entre onicofagia y manifestaciones clínicas de trastornos temporomandibulares en dentición mixta primera y/o segunda fase: Una revisión narrativa. Rev. Clin. Periodoncia Implantol. Rehabil. Oral. 2014;7(1):37- 42.
Lorente AA, Cortes O, Guzmán S, Vicente A, Garrido N. Oral Malocclusion and Its Relation to Nutritive and Non- nutritive Habits in School Children. Open J. Dent. Oral Medicine 2019;7(1):1-8.
Moss ML, Simon MR. Growth of the human mandibular angular process: A functional cranial analysis. Am. J. Phys. Antrophol. 1968;28(2):127-138.
Moss ML, Salentijn L. The primary role of functional matrices in facial growth. Am. J. Orthodontics 1969; 55(6):566-577.
Nakano H, Maki K, Shibasaki Y, Miller AJ. Three-dimensional changes in the condyle during development of an asymmetrical mandible in a rat: A microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2004;126(4):410-420.
Ma J, Wang J, Huang D et al. A comparative study of condyle position in temporomandibular disorder patients with chewing side preference using cone‐beam computed tomography. J Oral Rehabil 2022;49(2):265-271.
Luis J, Vergara M. Diferencias morfológicas y arquitecturales mandibulares en masticadores unilaterales [Internet]. 2006 [Consulted Nov 3, 2022 Available at: https://repositorio.uchile.cl/bitstream/handle/2250/140582/Diferencias-morfológicas- y-arquitecturales-mandibulares-en- masticadores-unilaterales.pdf?sequence=1
Planas P. Rehabilitación Neuro-Oclusal (RNO). 2nd ed. Strasbourg. Amolca; 2008.
Veli I, Uysal T, Ozer T, Ucar FI, Eruz M. Mandibular asymmetry in unilateral and bilateral posterior crossbite patients using cone-beam computed tomography. Angle Orthod. 2011;81(6):966-974.
Jiménez-Silva A, Peña-Durán C, Lee-Muñoz X, Vergara-Núñez C, Tobar-Reyes J, Frugone-Zambra R. Patología temporomandibular asociada a masticación unilateral en adultos jóvenes. Rev. Clin. Periodoncia Implantol. Rehabil. Oral 2016;9(2):125- 131.
Martinez-Gomis J, Lujan-Climent M, Palau S, Bizar J, Salsench J, Peraire M. Relationship between chewing side preference and handedness and lateral asymmetry of peripheral factors. Arch. Oral Biol. 2009;54(2):101-107.
Flores-Orozco EI, Rovira-Lastra B, Peraire M, Salsench J, Martinez-Gomis
J. Reliability of a visual analog scale for determining the preferred mastication side. J Prosthet Dent 2016;115(2):203- 208.
Diernberger S, Bernhardt O, Schwahn C, Kordass B. Self-reported chewing side preference and its associations with occlusal, temporomandibular and prosthodontic factors: results from the population-based Study of Health in Pomerania (SHIP-0). J Oral Rehabil 2008;35(8):613-620.
Facal García A. Diagnóstico y tratamiento precoz de las alteraciones funcionales del desarrollo craneofacial. Ortod Esp. 2006;46(3):79-200.
Larato DS. Effects of unilateral mastication on tooth and periodontal structures. J. Oral Med. 1970;25(3):80- 83.
Takada J, Miyamoto JJ, Yokota T, Ono T, Moriyama K. Comparison of the mandibular hinge axis in adult patients with facial asymmetry with and without posterior unilateral crossbite. Eur. J. Orthod 2015;37(1):22-27.
Talapaneni AK, Nuvvula S. The association between posterior unilateral crossbite and craniomandibular asymmetry: A systematic review. J Orthod 2012;39(4):279-291.
Facal García A. Clase II. Forma, función, desarrollo y estabilidad. Expoorto 09. 1st edition Several authors. Editorial Ripano S.A., D. L. 2009:149-168.
Iodice G, Danzi G, Cimino R, Paduano S, Michelotti A. Association between posterior crossbite, skeletal, and muscle asymmetry: a systematic review. Eur J Orthod 2016;38(6):638-651.
Thilander B, Bjerklin K. Posterior crossbite and temporomandibular disorders (TMDs): need for orthodontic treatment? Eur J Orthod 2011;34(6):667- 673.
Anhoury PS. Nonsurgical treatment of an adult with mandibular asymmetry and unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 2009;135(1):118-126.
Proffit WR. Contemporary Orthodontics. 2nd ed. Michigan. Mosby-Year Book; 1993.
Del Pinal Luna I, Molinero Mourelle P, Torres Loreta L, Bartolomé Villar
B. Tratamiento precoz de la mordida cruzada posterior unilateral en el paciente infantil. Bibliographic review. CIENT. DENT. 2015;12(3):41-48.
Kwak Y, Jang I, Choi D, Cha B. Functional evaluation of orthopedic and orthodontic treatment in a patient with unilateral posterior crossbite and facial asymmetry. Korean J Orthod. 2014;44(3):143-153.
Mata J, Zambrano F, Quirós O, Farias M, Rondón S, Lerner H. Expansión Rápida de Maxilar en Maloclusiones Transversales: Bibliographic review [Internet]. 2007 [accessed 12 Apr 2023]. Available at: https://www. ortodoncia.ws/publicaciones/2007/art- 11/
Haralur SB, Majeed MI, Chaturvedi S, Alqahtani NM, Alfarsi M. Association between preferred chewing side and dynamic occlusal parameters. J. Int. Med. Res 2019;47(5):1908-1915.
Nissan J, Gross MD, Shifman A, Tzadok L, Assif D. Chewing side preference as a type of hemispheric laterality. J Oral Rehabil 2004;31(5):412-416.
Christensen LV, Radue JT. Lateral preference in mastication: a feasibility study. J Oral Rehabil 1985;12(5):421- 427.
Tay DK. Physiognomy in the classification of individuals with a lateral preference in mastication. J. Orofac. Pain 1994;8(1):61-72.
Pond LH, Barghi N, Barnwell GM. Occlusion and chewing side preference. J Prosthet Dent 1986;55(4):498-500.
Wilding RJC, Adams LP, Lewin A. Absence of association between a preferred chewing side and its area of functional occlusal contact in the human dentition. Arch. Oral Biol. 1992;37(5):423-438.
Moss ML, DDS. Functional analysis of human mandibular growth. J Prosthet Dent 1960;10(6):1149-1159.
Rogers WM. The influence of asymmetry of the muscles of mastication upon the bones of the facer. Anat. 1958;131(4):617-632.
Legrell PE, Isberg A. Mandibular length and midline asymmetry after experimentally induced temporomandibular joint disk displacement in rabbits. Am J Orthod Dentofacial Orthop. 1999;115(3):247.
Legrell PE, Isberg A. Mandibular height asymmetry following experimentally induced temporomandibular joint disk displacement in rabbits. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;86(3):280-285.
Marqués Junior JA, J. Lenci PR. Consecuencias de la masticación unilateral en el desarrollo y equilibrio del sistema estomatognático [Internet]. [Accessed 16 Apr 2023]. Available at:http://www.labiela.net/La%20 Biela01/01jm2.htm
Harvold EP, Francisco C. The role of function in the etiology and treatment of malocclusion.Am. J. Orthod. 1968;54(12):883-898.
Ma J, Wang J, Huang D et al. A comparative study of condyle position in temporomandibular disorder patients with chewing side preference using cone‐beam computed tomography. J Oral Rehabil 2022;49(2):265-271.
Reinhardt R, Tremel T, Wehrbein H, Reinhardt W. The Unilateral Chewing Phenomenon, Occlusion, and TMD. Cranio 2006; 24(3):166-170.
Santana-Mora U, López-Cedrún J, Mora MJ, Otero XL, Santana-Penín U. Temporomandibular disorders: The habitual chewing side syndrome. PLoS One 2013;8(4):e59980. doi: 10.1371/journal.pone.0059980.
Jiang H, Li C, Wang Z et al. Assessment of osseous morphology of temporomandibular joint in asymptomatic participants with chewing- side preference. J Oral Rehabil 2015;42(2):105-112.
Hinton RJ. Changes in articular eminence morphology with dental function. Am. J. Phys. Anthropol. 1981;54(4):439-455.
Yashiro K, Iwata A, Takada K, Murakami S, Uchiyama Y, Furukawa S. Temporomandibular joint articulations on working side during chewing in adult females with crossbite and mandibular asymmetry. J Oral Rehabil 2015;42(3):163-172.
Eriksson L, Westesson PL, Macher D, Hicks D, Tallents RH. Creation of disc displacement in human temporomandibular joint autopsy specimens. J. Oral Maxillofac. Surg.1992 50(8):869-873.
Pullinger AG, Seligman DA, Gombein JA. A multiple logistic regression analysis of the risk and relative odds of temporomandibular disorders as a function of common occlusal features. J. Dent. Res 1993; 72(6):968-979.
Petrén S, Bondemark L, Söderfeldt B. A systematic review concerning early orthodontic treatment of unilateral posterior crossbite. Angle Orthod. 2003;73(5):588-596.
De Boer M, Steenks MH. Functional unilateral posterior crossbite. Orthodontic and functional aspects. J Oral Rehabil 1997;24(8):614-623.
Malandris M, Mahoney EK. Aetiology, diagnosis and treatment of posterior cross-bites in the primary dentition. Int J Paediatr Dent. 2004;14(3):155-166.
Brin I, Ben-Bassat Y, Blustein Y et al. Skeletal and functional effects of treatment for unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1996;109(2):173-179.
Petrén S, Bondemark L. Correction of unilateral posterior crossbite in the mixed dentition: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2008;133(6):790.e7-790.e13. doi.
org/10.1016/j.ajodo.2007.11.021.

Escobar Bores, Paloma
Graduated in Odontology Universidad CEU San Pablo Orthodontics collaborator in the Dentistry Department of the Faculty of Medicine of Universidad CEU San Pablo.
Peña Salguero, Paula María
Associate Professor of Orthodontics in the Odontology Department of the Medicine Faculty of Universidad CEU San Pablo. Odontology Degree in Universidad Rey Juan Carlos URJC. Master Degree in Orthodontics at Universidad de Alcalá de Henares UAH- CEPUME.
Arias Macías, Caridad
Director of the Odontology Department of Universidad CEU San Pablo.